A study published in this month’s AJSM (July 2018) compared the long term (17 year) outcomes between ACL reconstructions with BTB autograft and hamstring autograft. Graft choice for ACL surgery is an interesting topic in the sports medicine world. With the incidence of ACL ruptures continually increasing, this is a common injury seen by orthopedic sports surgeons and one that draws a lot of attention in the media. The question of ‘which graft?‘ comes up a lot in my practice, so I decided to use this article as the backbone for this latest blog post: graft choice in ACL surgery.
Graft choice in ACL surgery is a continual debate amongst patients and clinicians. Patients are continually asking for my opinion on which graft is best: the patella tendon (aka. BTB or “bone-tendon-bone”) or the hamstring tendons (…or maybe even an allograft?!). As with most choices in medicine, there are pros and cons to each side.
To cover this topic, let’s first take a step back. ACL grafts should first be broadly classified as either autografts or allografts. An autograft is a graft of tissue taken from the patient’s own body; an allograft is a graft from a human cadaver. In the young (< 35 years old), active patient cohort, there is strong evidence to support the use of an autograft for ACL reconstruction. Allograft tissue is associated with a significant higher failure rate (ie. the chance of the graft tearing and requiring revision surgery). The Westpoint trial by Pallis et al. (AJSM 2012) is one good example illustrating this point (allograft reconstructions were 7.7 times more likely to fail compared to autografts in this young, active cohort of military cadets). As a result, our practices around graft choice have changed over time, as shown here (Arthroscopy 2017), with a move away from the use of allografts in younger patients. This recent study by Maletis et al (AJSM 2017) is a good overview of the differences between auto- and allografts, while stratifying for the various allograft processing techniques which has been shown to influence failure rates in allografts (Background: Allograft tissue must be processed – irradiated and/or chemically washed – to decreased the risk of disease transmission prior to implantation in the recipient. This weakens the tissue. There are a variety of ways that allograft tissue is processed. Graft processing techniques have come under review in the literature recently in an attempt to decrease the failure rates associated with the various processing techniques).
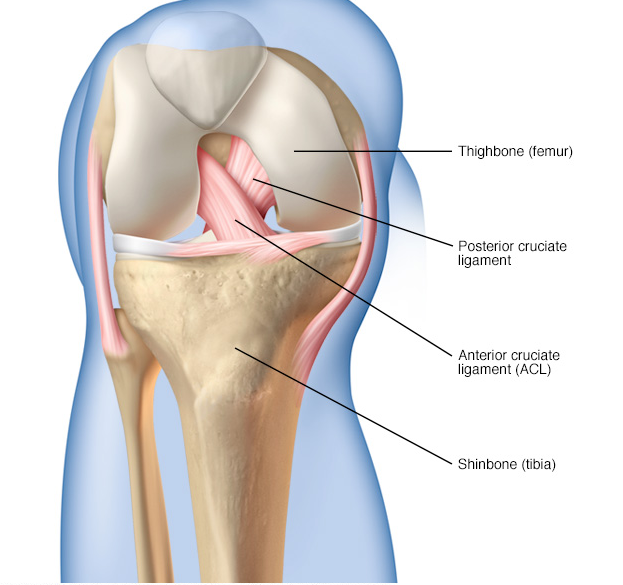
The problem with autografts is donor-site morbidity (as the saying goes, “robbing Peter to pay Paul”). Harvesting the graft tissue (ie. removing the central third of the patella tendon or the two hamstring tendons – semitendinosus and gracilis – to reconstruct the ACL) sometimes causes pain or potential complications after the surgery or at some point down the line (ex. anterior knee pain or kneeling pain after BTB graft harvest or knee flexion weakness after hamstring harvest). However, the significantly higher failure rate of allografts is tough to overlook. Their potential benefit (or rather the benefit of avoiding the possible morbidity of autograft harvest) is far outweighed by their significantly higher failure rate, in my opinion.
So, for most young patients, the question is not deciding between an auto- or allograft, but rather which autograft: BTB or hamstring. Unfortunately (or, perhaps, fortunately), the debate between BTB and hamstring autografts is not as clear cut: the literature would suggest that they are both equally as good (ie. the functional outcomes are equivalent in most studies). Yes, there are specific pros and cons to each graft, but most of the literature shows equal functional outcomes between the two. Here is a three-point summary of the large majority of data published comparing the two techniques (and there has been a lot of literature published!):
- BTB grafts are more likely to restore objective stability in the knee (in other words, residual knee laxity is more common with hamstring grafts, especially in females).
- BTB grafts are associated with more post-operative donor site morbidity (ex. anterior knee pain and kneeling pain) and have a greater risk of post-operative arthritis at long term follow-up. (It should also be noted that BTB autografts are generally associated with more pain in the immediate post-operative period, as shown here).
- In terms of functional outcomes and graft failure, there is no significant difference between the two grafts.
A study published in this month’s AJSM compared the long term (17 year) outcomes between ACL reconstructions with BTB autograft and hamstring autograft. This was a follow-up study from the same group’s 5 year and 11 year follow up papers. At the 17-year follow-up, no statistically significant differences were seen with respect to graft failure and functional outcome. Interestingly, patients who had undergone reconstruction with a BTB were more likely to have osteoarthritis in their knee. Furthermore, 100% of the BTB patients had some degree of arthritis in their knee (compared to 71% in the hamstring group).
Overall, the graft choice decision should be individualized to the patient. Risks and benefits of each graft should be discussed in detail and the patient and doctor should arrive at the decision together, only after all options are considered. In younger, active patients, it’s my recommendation to avoid allografts (this is strongly supported in the literature).
In an attempt to summarize most of the data (for anyone interested!), I’ve grouped the individual papers that compare the results between BTB and hamstring autografts for ACL reconstruction:
Studies showing near equivalent outcomes between hamstring and BTB autografts:
- Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. (Cochrane Database Systematic Review, 2011).
- A Randomized Clinical Trial Comparing Patellar Tendon, Hamstring Tendon, and Double-Bundle ACL Reconstructions: Patient-Reported and Clinical Outcomes at a Minimal 2-Year Follow-up. (Clin J Sport Med, 2015).
- A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. (Knee, 2015).
- A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone-patellar tendon-bone autografts for the reconstruction of the anterior cruciate ligament. (Arch Orthop Trauma Surg, 2012).
- Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. (Arthroscopy, 2005).
- A comparison of ACL reconstruction using patellar tendon versus hamstring autograft in female patients: a prospective randomised study. (Int Orthop, 2015).
- Knee Osteoarthritis After Anterior Cruciate Ligament Reconstruction With Bone-Patellar Tendon-Bone Versus Hamstring Tendon Autograft: A Systematic Review of Randomized Controlled Trials. (Arthroscopy, 2018).
- Bone-Patellar Tendon-Bone Versus Hamstring Tendon Autografts for Primary Anterior Cruciate Ligament Reconstruction: A Systematic Review of Overlapping Meta-analyses. (Orthop J Sport Med, 2017).
- Comparison of hamstring and patellar tendon grafts in anterior cruciate ligament reconstruction: A prospective randomized study. (J Int Med Red, 2018).
- Long-Term Outcomes in Anterior Cruciate Ligament Reconstruction: A Systematic Review of Patellar Tendon Versus Hamstring Autografts. (Orthop J Sports Med, 2017).
- Anatomic Anterior Cruciate Ligament Reconstruction via Independent Tunnel Drilling: A Systematic Review of Randomized Controlled Trials Comparing Patellar Tendon and Hamstring Autografts. (Arthroscopy, 2017).
- Outcome of Patellar Tendon Versus 4-Strand Hamstring Tendon Autografts for Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis of Prospective Randomized Trials. (Arthroscopy, 2017).
- A Randomized Controlled Trial With Mean 16-Year Follow-up Comparing Hamstring and Patellar Tendon Autografts in Anterior Cruciate Ligament Reconstruction. (Am J Sports Med, 2016).
- Knee stability after arthroscopic anterior cruciate ligament reconstruction using the middle third of the patellar ligament and quadrupled hamstring tendons grafts – A two-year follow-up. (Injury, 2015).
- Comparison of Patellar Tendon and Hamstring Tendon Anterior Cruciate Ligament Reconstruction: A 15-Year Follow-up of a Randomized Controlled Trial. (Am J Sports Med, 2016).
- Primary anterior cruciate ligament reconstruction in athletes: a 5-year follow up comparing patellar tendon versus hamstring tendon autograft. (Wien Klin Wochenschr, 2015).
- A two- and five-year follow-up of clinical outcome after ACL reconstruction using BPTB or hamstring tendon grafts: a prospective intervention outcome study. (Knee Surg Sports Traumatol Arthrosc, 2015).
- Long-term follow-up of patellar tendon grafts or hamstring tendon grafts in endoscopic ACL reconstructions. (Knee Surg Sports Traumatol Arthrosc, 2013).
- Knee function after anterior cruciate ligament reconstruction with patellar or hamstring tendon: a meta-analysis. (Chin Med J, 2011).
- Anterior cruciate ligament reconstruction using patellar tendon versus hamstring tendon: a prospective comparative study with 9-year follow-up. (Arthroscopy, 2011).
- No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. (Am J Sports Med, 2010).
- Patellar tendon versus hamstring tendon autografts for anterior cruciate ligament reconstruction: a randomized controlled trial using similar femoral and tibial fixation methods. (Am J Sports Med, 2009).
- Knee laxity measurements after anterior cruciate ligament reconstruction, using either bone-patellar-tendon-bone or hamstring tendon autografts, with special emphasis on comparison over time. (Knee Surg Sports Traumatol Arthrosc, 2009).
- Osteoarthritic changes after anterior cruciate ligament reconstruction using bone-patellar tendon-bone or hamstring tendon autografts: a retrospective, 7-year radiographic and clinical follow-up study. (Arthroscopy, 2008).
- A prospective comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction in female patients. (Knee Surg Sports Traumatol Arthrosc, 2006).
- Comparing 2-year outcomes of anterior cruciate ligament reconstruction using either patella-tendon or semitendinosus-tendon autografts: a non-randomised prospective study. (J Orthop Surg (Hong Kong), 2005).
- Patellar tendon or four-strand hamstring? A systematic review of autografts for anterior cruciate ligament reconstruction. (Knee, 2005).
- Anterior cruciate ligament reconstruction, hamstring versus bone-patella tendon-bone grafts: a systematic literature review of outcome from surgery. (Knee, 2005).
- A prospective randomized comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction. (Arthroscopy, 2005).
- Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring: does it really matter? A systematic review. (Am J Sports Med, 2004).
- Arthroscopically assisted anterior cruciate ligament reconstruction: comparison of bone-patellar tendon-bone versus hamstring tendon autograft. (J Med Assoc Thai, 2004).
- Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. (J Bone Joint Surg Am, 2004).
- A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. (Am J Sports Med, 2003).
- Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction? A prospective randomized study with a two-year follow-up. (Am J Sports Med, 2003).
- A prospective randomized study of patellar versus hamstring tendon autografts for anterior cruciate ligament reconstruction. (Am J Sports Med, 2003).
- A five-year comparison of patellar tendon versus four-strand hamstring tendon autograft for arthroscopic reconstruction of the anterior cruciate ligament. (Am J Sports Med, 2002).
- A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. (Am J Sports Med, 2002).
- Four-strand hamstring tendon autograft compared with patellar tendon-bone autograft for anterior cruciate ligament reconstruction. A randomized study with two-year follow-up. (Am J Sports Med, 2001).
- Arthroscopy-assisted anterior cruciate ligament reconstruction with patellar tendon or hamstring autografts. Bull Hosp Jt Dis, 2000).
- Arthroscopic reconstruction of the anterior cruciate ligament. A comparison of patellar tendon autograft and four-strand hamstring tendon autograft. (Am J Sports Med, 1999).
Studies supporting BTB autografts:
- Increased knee laxity with hamstring tendon autograft compared to patellar tendon autograft: a cohort study of 5462 patients with primary anterior cruciate ligament reconstruction. (Knee Surg Sports Traumatol Arthrosc, 2018).
- Graft failure is more frequent after hamstring than patellar tendon autograft. (Knee Surg Sports Traumatol Arthrosc, 2018).
- Bone-patellar tendon-bone autograft could be recommended as a superior graft to hamstring autograft for ACL reconstruction in patients with generalized joint laxity: 2- and 5-year follow-up study. (Knee Surg Sports Traumatol Arthrosc, 2018).
- Comparison of Return to Pre-Injury Sport After 10 mm Size Bone-Patellar Tendon-Bone (BPTB) versus 8 mm Hamstring Anterior Cruciate Ligament Reconstruction: A Retrospective Study with a Two-Year Follow-Up. (Med Sci Monit, 2018).
- Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. (Am J Sports Med, 2014).
- Bone-Patellar Tendon-Bone Autograft versus Hamstring Tendon Autograft for Anatomical Anterior Cruciate Ligament Reconstruction with Three-Dimensional Validation of Femoral and Tibial Tunnel Positions. (J Knee Surg, 2017).
- Compensation after treatment for anterior cruciate ligament injuries: a review of compensation claims in Norway from 2005 to 2015. (Knee Surg Sports Traumatol Arthrosc, 2018).
- Incidence of Second Anterior Cruciate Ligament Tears (1990-2000) and Associated Factors in a Specific Geographic Locale. (Am J Sports Med, 2017).
- Hamstring Autograft versus Patellar Tendon Autograft for ACL Reconstruction: Is There a Difference in Graft Failure Rate? A Meta-analysis of 47,613 Patients. (Clin Orthop Relat Res, 2017).
- Autograft Choice in Young Female Patients: Patella Tendon versus Hamstring. (J Knee Surg, 2017).
- Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. (Am J Sports Med, 2014).
- Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the danish registry of knee ligament reconstruction. (Am J Sports Med, 2014).
- Reconstruction of the anterior cruciate ligament: association of graft choice with increased risk of early revision. (Bone Joint J, 2013).
- A 2-year follow-up of rehabilitation after ACL reconstruction using patellar tendon or hamstring tendon grafts: a prospective randomised outcome study. (Knee Surg Sports Traumatol Arthrosc, 2010).
- Patellar tendon versus hamstring tendon autografts for reconstructing the anterior cruciate ligament: a meta-analysis based on individual patient data. (Am J Sports Med, 2009).
- Knee extension and flexion muscle power after anterior cruciate ligament reconstruction with patellar tendon graft or hamstring tendons graft: a cross-sectional comparison 3 years post surgery. (Knee Surg Sports Traumatol Arthrosc, 2009).
- A prospective comparison of bone-patellar tendon-bone and hamstring tendon grafts for anterior cruciate ligament reconstruction in male patients. (Knee Surg Sports Traumatol Arthrosc, 2007).
- Joint laxity and isokinetic thigh muscle strength characteristics after anterior cruciate ligament reconstruction: bone patellar tendon bone versus quadrupled hamstring autografts. (Clin J Sport Med, 2006).
- Quantitative evaluation of anterior tibial translation during isokinetic motion in knees with anterior cruciate ligament reconstruction using either patellar or hamstring tendon grafts. (Int Ortho, 2005).
- Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. (Am J Sports Med, 2003).
- Anterior cruciate ligament replacement: comparison of bone-patellar tendon-bone grafts with two-strand hamstring grafts. A prospective, randomized study. (J Bone Joint Surg Am, 2002).
- Reconstruction of the anterior cruciate ligament in females: A comparison of hamstring versus patellar tendon autograft. (Arthroscopy, 2002).
- Patellar versus hamstring tendons in anterior cruciate ligament reconstruction: A meta-analysis. (Arthroscopy, 2001).
- Tunnel expansion following anterior cruciate ligament reconstruction: a comparison of hamstring and patellar tendon autografts. (Knee Surg Sports Traumatol Arthrosc, 1997).
Studies supporting Hamstring autografts:
- Hamstring tendon versus patellar tendon anterior cruciate ligament reconstruction using biodegradable interference fit fixation: a prospective matched-group analysis. (Am J Sports Med, 2005).
- Increased incidence of osteoarthritis of knee joint after ACL reconstruction with bone-patellar tendon-bone autografts than hamstring autografts: a meta-analysis of 1,443 patients at a minimum of 5 years. (Eur J Orthop Surg Traumatol, 2015).
- Comparison of patellar versus hamstring tendon autografts in arthroscopic anterior cruciate ligament reconstruction: A 6-month follow-up of a randomized clinical trial. (J Res Med Sci, 2017).
- Twenty-Year Outcome of a Longitudinal Prospective Evaluation of Isolated Endoscopic Anterior Cruciate Ligament Reconstruction With Patellar Tendon or Hamstring Autograft. (Am J Sports Med, 2016).
- Bone-patellar tendon-bone autograft versus hamstring autograft anterior cruciate ligament reconstruction in the young athlete: a retrospective matched analysis with 2-10 year follow-up. (Knee Surg Sports Traumatol Arthrosc, 2012).
- Hamstring tendon autograft better than bone patellar-tendon bone autograft in ACL reconstruction: a cumulative meta-analysis and clinically relevant sensitivity analysis applied to a previously published analysis. (Acta Orthop, 2007).
- Overlapping systematic reviews of anterior cruciate ligament reconstruction comparing hamstring autograft with bone-patellar tendon-bone autograft: why are they different? (J Bone Joint Surg Am, 2007).
- A 6-year follow-up of the effect of graft site on strength, stability, range of motion, function, and joint degeneration after anterior cruciate ligament reconstruction: patellar tendon versus semitendinosus and Gracilis tendon graft. (Am J Sports Med, 2007).
- A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. (Am J Sports Med, 2007).
- Anterior cruciate ligament reconstruction in females: a comparison of hamstring tendon and patellar tendon autografts. (Knee Surg Sports Traumatol Arthrosc, 2006).