Runner’s knee is probably one of the more confusing topics in sports medicine, largely because most people don’t really know what it is. Or even if they do know what it is, they don’t understand how it works. For me, if you can get your head around the underlying cause, you can understand how to treat the problem. Yes – I understand how cliché-ish this sounds, but Runner’s Knee really is the mystery of knee problems for a lot of people (patients and clinicians!). Believe me, most people don’t really know what it is! The good news is that it truly is a simple problem and if you can understand the underlying pathoanatomy, you’ll be able to successfully treat the condition and resolve your nagging knee pain.
Runner’s knee is the common term for the medical condition known as patellofemoral syndrome (aka. patellofemoral pain syndrome or anterior knee pain) – similar to “tennis elbow” for lateral epicondylitis, although not as straightforward. The radiologic term for this condition, further adding to its complexity, is called “chondromalacia patellae”. Let’s take a step back and explain (read: simplify) these confusion terms.
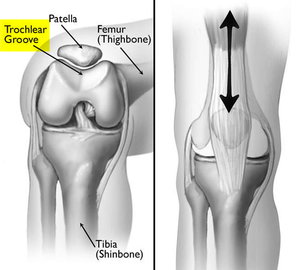
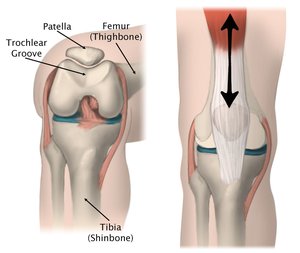
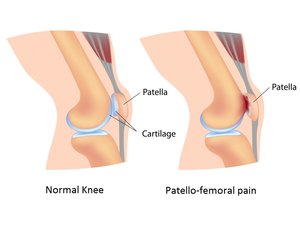
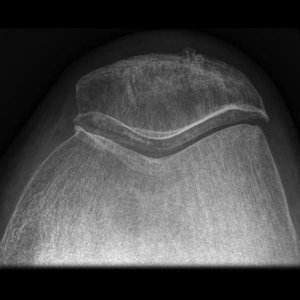
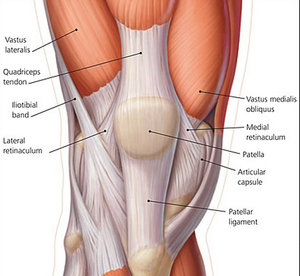
The front of the knee (anterior = front) is composed of the patellofemoral joint. The patella (or kneecap) sits in a shallow groove in the front of the thigh bone (femur) known as the trochlear groove (patella + femur = patellofemoral joint). The patella links the quads tendon with the patella tendon. It functions primarily as an anatomic pulley for the quadriceps muscle and increases the lever arm of the extensor mechanism allowing for more effective knee extension (simply put, it allows the quadriceps muscle to function more effectively to straighten the leg). Hyaline cartilage lines both the under surface of the patella and the surface of the trochlear groove (side note: the patella cartilage is the thickest cartilage in the human body, for good reason). “Chondromalacia” (translation: “Sick cartilage”) is an aliment of the hyaline cartilage coating of the articular surface of a bone (in this case, the undersurface of the patella). It results in softening, fissuring, and erosion of the hyaline cartilage (remember, erosion and loss of the articular cartilage coating of a joint is more commonly called arthritis). Chondromalacia of the undersurface of the patella is diagnosed on an MRI and referred to as chondromalacia patella – again, this is the radiographic term for patellofemoral syndrome. Because it is so common, chondromalacia of the patella has been given its own name!
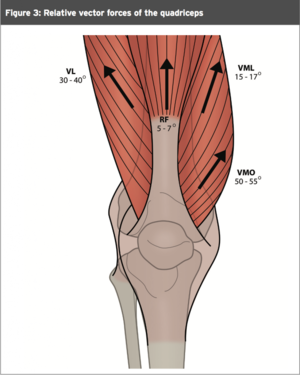
So, what causes the softening and fissuring of the undersurface of the patella (and the pain that this brings)? Patellofemoral syndrome is an abnormality in the tracking of the patella in the femoral or trochlear groove. The patella may, in some cases, be tracking in the central aspect of the trochlea where it should, however, the pressure within the joint may be abnormality elevated due to a subtle imbalance in the muscles that control this joint (the quads in the front and the hamstrings in the back). Alternatively, the alignment across the knee may be subtly altered, leading to patella maltracking within the trochlea. In other words, the patella doesn’t track or slide directly in the middle of the groove. Rather, it tracks and rubs against the slide of the groove. In most cases, because of the valgus alignment across the read (valgus = “knocked-knees”; normally, the angle between the femur and tibia is roughly 7 degrees valgus), the patella is pulled slightly laterally (towards the outside). This will produce pain in the outside of the knee that is worse with repetitive flexion exercises like running or squatting.
Simply put, patellofemoral syndrome is caused by elevated stress and friction within the patellofemoral joint, which cause inflammation and damage to the cartilage within the joint. Therefore, if you can identify and understand the cause of this increased friction, you will be able to correct the problem and stop the pain (and yes, this condition is very treatable by conservative measures).
In most cases, the cause of the increased pressure within the patellofemoral joint is a subtle imbalance between the knee flexors (hamstrings) and the knee extensors (quads). Typically, the hamstrings are too tight (or strong), relative to the quads (tight hamstrings function to pull the tibia back. Since the patella tendon is attached to the front of the tibia, this effectively increases the pressure within the patellofemoral joint). The correction, in this case, is obvious: strengthen the quads and stretch the hamstrings. When the patella is tracking laterally, causing friction, inflammation, and pain that is focused in the lateral aspect of the knee, the correction is to strength the medial muscles to help pull the patella back to the inside so that it slides in the center of the trochlear groove, rather than on the outside. Exercises should focus on strengthening the medial muscles, specifically vastus medialis obliquus (VMO).
Overall, the treatment for runner’s knee without any structural abnormality is entirely conservative and should address the functional causes. Physical therapy should be aimed at correcting the underlying abnormality that is responsible for either the maltracking of the patella or the increased pressure within the joint. An MRI is typically not necessary; it is usually done to rule out other causes of pain (ex. meniscal injuries) and in most cases it is entirely normal (other than the common suggestion of chondromalacia patellae). Injections can be used to treat the inflammation within the knee joint and offer the patient some relief to help in physical therapy. But, it is important to remember that an injection will not correct the underlying issue that is causing the problem. Injection therapies include platelet-rich plasma (PRP) and corticosteroids and the risks and benefits of each should be discussed with the patient in detail.
Articles for further reading:
- Patellofemoral pain syndrome. (KSSTA 2014).
- Patellofemoral pain in athletes. (J Sports Med 2017).
- Study protocol: a randomised controlled trial comparing the long term effects of isolated hip strengthening, quadriceps-based training and free physical activity for patellofemoral pain syndrome (anterior knee pain). (BMC Musculoskelet Disord 2015).
- A review of the management of patellofemoral pain syndrome. (Phys Sportsmed 2013)
- Does the Addition of Hip Strengthening to a Knee-Focused Exercise Program Improve Outcomes in Patients With Patellofemoral Pain Syndrome? (J Sport Rehabil 2015)
- Patellofemoral pain syndrome: a review on the associated neuromuscular deficits and current treatment options. (Br J Sports Med 2008).
- Closed kinetic chain exercises with or without additional hip strengthening exercises in management of patellofemoral pain syndrome: a randomized controlled trial. (Eur J Phys Rehabil Med 2013)
Muscle Above Knee Leg Muscle Over Knee Knee Pain Right Above Knee – Human Anatomy – ANATOMY HUMAN PARTS