Definition
Adhesive capsulitis, more commonly referred to as “frozen shoulder”, is a poorly defined syndrome. However, most can agree that adhesive capsulitis is characterized by the restriction or loss of both passive and active range of motion (ROM) without an osseous basis for this limitation due to soft tissue contracture of the glenohumeral joint. Shoulder stiffness can be caused by tissue scarring or intra-articular, subacromial, and/or subdeltoid adhesions, as well as changes in the osseous structures of the shoulder. The key component to recognize adhesive capsulitis is the loss of range of motion, primarily passive external rotation, of the glenohumeral joint. One exception to this key component is calcific tendonitis, which may be distinguished from adhesive capsulitis on a plain radiograph.
Adhesive capsulitis is broken down into two forms:
- Primary Adhesive Capsulitis (Idiopathic)
- Secondary Adhesive Capsulitis:
– Intrinsic: Corresponding with rotator cuff disorders, biceps tendinitis, calcific tendinitis, previous shoulder surgery, and proximal humerus fracture.
– Extrinsic: Problematic occurrence extrinsic to the glenohumeral joint such as a previous ipsilateral breast surgery, cervical radiculopathy, previous fracture of the shoulder, acromioclavicular joint arthritis, clavicular fracture, or a scapulothoracic abnormality.
– Systemic: Corresponding with disorders such as diabetes mellitus, hyperthyroidism, hypothyroidism, hypoadrenalism, or myocardial infarction. Systemic adhesive capsulitis is most commonly associated with diabetes mellitus, and rarely these other conditions listed.
Anatomy
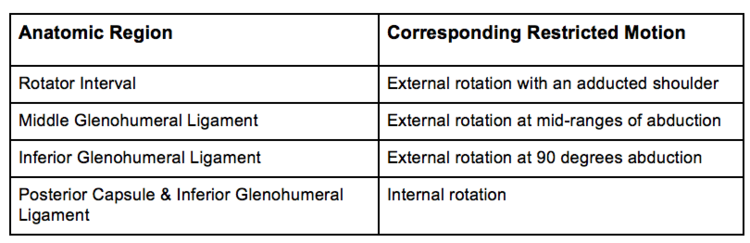
The motion of the shoulder is executed primarily at the articulation in the glenohumeral joint and scapulothoracic joint. The ratio of motion between the two articulations is 2:1, respectively. Capsuloligamentous structures are accredited with providing stability to the shoulder joint. Within the capsule are ligaments that provide support: the superior glenohumeral ligament, the coracohumeral ligament, the middle glenohumeral ligament, and the inferior glenohumeral ligament complex. The inferior glenohumeral ligament complex is comprised of the anterior band, axillary fold, and the posterior band. The superior glenohumeral ligament and coracohumeral ligament are located in the triangular shaped region, called the rotator interval, that lies between the anterior border of the supraspinatus tendon and the superior border of the subscapularis. During rotator cuff lengthening and shortening, these ligaments are tightened and loosened. Specific restrictions or loss of range of motion correspond to the contractures of the capsule regions and ligaments.
Contractures of the Capsuloligamentous Region & Correlation to Shoulder Motion:
Pathogenesis
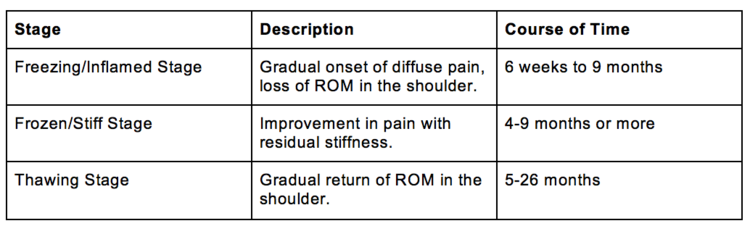
Adhesive capsulitis is most commonly seen in women and in patients between the ages of 40 and 60. Clinically, the disorder is categorized into three different stages:
Natural History
The time course and final results are widely variable in adhesive capsulitis. There is also a weak correlation between pain and a restricted ROM. Some patients experience a very restricted ROM accompanied with no pain, while others experience normal ROM with significant shoulder pain. However, the impact that the restricted ROM will produce greatly depends on the patient’s functional demands. Adhesive capsulitis is more resistant to a nonoperative approach when it occurs in systemic cases, such as diabetes mellitus.
Patient History
Although patients with adhesive capsulitis deny a traumatic event, secondary adhesive capsulitis is often a result of trauma, surgery, or medical comorbidities. One should take note of previous fractures, extended immobilization, previous surgeries, diabetes mellitus, and thyroid disorders. Important surgeries to take note of include a prior rotator cuff repair, capsular shift, Putti-Platt, Bristow-Latarjet, open glenoid grafting, and ORIF (open reduction and internal fixation) of a fracture around the shoulder. Other symptoms that could be expressed by the patient are acromioclavicular (AC) joint pain, periscapular pain, radicular deltoid pain, and a painful arc motion.
Physical Exam
A physician may utilize the following in their diagnosis:
- Bilateral passive ROM examination tests
- Assessment of the anterosuperior capsule: Indicated by a loss of passive external rotation in adduction.
- Assessment of the anteroinferior capsule: Indicated by a loss of passive external rotation with abduction of the arm.
- Assessment of the inferior capsule: Indicated by a loss of passive flexion and abduction.
- Assessment of the posterior capsule: Indicated by a loss of passive internal rotation.
Furthermore, the shoulder may be examined for signs of trauma, past surgeries and deformities. Other tests such as manual motor testing, passive and active ROM testing, ROM testing in the supine position, and the Lidocaine intra-articular injection test may be performed to help make an accurate diagnosis.
Imaging/Diagnostics
Disuse osteopenia, calcific tendinitis, fractures, arthritis, and surgical hardware can be identified through routine radiographs in the anteroposterior (AP) view, neutral, internal and external rotation views, and the Y and axillary lateral views. An MRI (magnetic resonance imaging) is ordered only in the event of a suspected rotator cuff or soft tissue injury. The loss of axillary recess on an MR Arthrogram typically indicates contracture of the joint capsule which can be associated with adhesive capsulitis.
Differential Diagnosis
- Glenohumeral Arthritis
- Acromioclavicular Arthritis
- Rotator Cuff Tendinitis
- Subacromial or Subdeltoid Bursitis
- Bicipital Tendinitis
- Calcific Tendinitis
- Septic Arthritis
- Rotator Cuff Tears
- Gout or crystalline arthropathy
- Cervical Radiculopathy
- Thoracic Outlet Syndrome
Nonoperative Treatment
A nonoperative approach is typically the first line of treatment in most cases. It is best utilized in patients with primary or secondary adhesive capsulitis within a time period of four to six months that have yet to have any treatment. Nonsteroidal anti-inflammatories (NSAIDs), physical therapy, and intra-articular steroid injections form the basis of a conservative management approach. This approach is successful in most cases, however the patient needs to understand the natural history and time course of the disorder. The most common complication is decreased range of motion compared to the contralateral shoulder.
Surgical Management
Surgery is not the best option for early-stage adhesive capsulitis. In fact, surgery should be avoided during the “freezing stage” as it may limit ROM that could potentially be recovered nonoperatively. The primary indication for surgery in adhesive capsulitis is a failure to improve with an extensive course of conservative management, including NSAIDs, a organized course of physical therapy, and intra-articular steroid injections. Surgery consists of a manipulation under anesthesia followed by an arthroscopic lysis of adhesions and release of the rotator interval (anterior capsule).
If you are suffering from a stiff, painful (possibly frozen) shoulder, contact Dr. Dold for an appointment today! 469.850.0680
Clinical Studies
- Optimal dose of intra-articular corticosteroids for adhesive capsulitis: a randomized, triple-blind, placebo-controlled trial. AJSM 2013.
- Intraarticular corticosteroids, supervised physiotherapy, or a combination of the two in the treatment of adhesive capsulitis of the shoulder: a placebo-controlled trial. Arthritis Rheum 2003.
- A randomized controlled trial of intra-articular triamcinolone and/or physiotherapy in shoulder capsulitis. Rheumatology 2005.
- Adhesive capsulitis of the shoulder. JAAOS 2011.
- The natural history of idiopathic frozen shoulder: a 2- to 27-year followup study. CORR 2012.
- Motion and pain relief remain 23 years after manipulation under anesthesia for frozen shoulder. CORR 2013.
- Comparison of manipulation and arthroscopic capsular release for adhesive capsulitis: a systematic review. JSES 2013.
- Short-term outcomes after arthroscopic capsular release for adhesive capsulitis. JSES 2016.
- Long-term outcomes after arthroscopic capsular release for idiopathic adhesive capsulitis. JBJS 2012.
- The diabetic frozen shoulder: arthroscopic release. Arthroscopy 1997.
- Comparison of arthroscopic capsular release in diabetic and idiopathic frozen shoulder patients. Arch Orthop Trauma Surg 2010.
- Thawing the frozen shoulder: the “patient” patient. Orthopedics 1996.
- Gentle thawing of the frozen shoulder: a prospective study of supervised neglect versus intensive physical therapy in seventy-seven patients with frozen shoulder syndrome followed up for two years. JSES 2004.
- Manual therapy and exercise for adhesive capsulitis (frozen shoulder). Cochrane Database Review 2014.
- Thawing the frozen shoulder. A randomised trial comparing manipulation under anaesthesia with hydrodilatation. JBJS 2007.
- Platelet-rich plasma injection in the treatment of frozen shoulder: A randomized controlled trial with 6-month follow-up . Int J Clin Pharmacol Ther 2018.
- Idiopathic adhesive capsulitis. A prospective functional outcome study of nonoperative treatment. JBJS 2000.
- Good results after fluoroscopic-guided intra-articular injections in the treatment of adhesive capsulitis of the shoulder. Knee Surg Sports Traumatol Arthrosc 2010.
- The resistant frozen shoulder: Manipulation versus arthroscopic release. Clin Orthop Relat Res 1995.
- Is the extended release of the inferior glenohumeral ligament necessary for frozen shoulder? Arthroscopy 2010.


