Definition
Glenohumeral arthritis (more commonly known as shoulder arthritis) is defined as the loss of articular cartilage within the shoulder joint. The shoulder joint is made up of the humeral head and the shallow glenoid fossa of the scapula. Soft tissue contractures, rotator cuff dysfunction, and bone erosion often accompany arthritis of the shoulder and are important considerations when deciding on an appropriate treatment plan. When dealing with an arthritic shoulder it is vital to consider the integrity of the rotator cuff; the outcome of surgery is greatly dependent on the integrity or reparability of the rotator cuff. Conditions such as osteoarthritis, posttraumatic arthritis, and avascular necrosis are usually associated with an intact or reparable rotator cuff. However, rotator cuff arthropathy, a unique form of glenohumeral arthritis, only occurs in the context of a large, irreparable rotator cuff tear. Other conditions, including inflammatory arthritides, may also been associated with a non-functional cuff and is an important consideration for surgery.

XRay illustrating advanced, end-stage osteoarthritis of the glenohumeral (shoulder) joint.
Pathogenesis
In most cases, the specific cause of glenohumeral arthritis is unknown, termed primary or idiopathic osteoarthritis. However, the loss of articular cartilage may be associated with previous trauma or fractures of the joint (post-traumatic arthritis), avascular necrosis, or various autoimmune or inflammatory conditions affecting the shoulder (ex. rheumatoid arthritis). Primary osteoarthritis may be related to anatomic factors such as glenoid hypoplasia or increased retroversion, but for most patients no cause is evident. In avascular necrosis (AVN), arthritis results after collapse of the humeral head. Involvement of glenoid articular cartilage does not occur until the later stages of the disease when the irregular humeral head has been articulating with the previously normal glenoid surface. Rheumatoid arthritis (RA) is caused by the immune system activating and releasing excessive lymphocytes into the joint and synovial tissue. Cytokines, destructive enzymes, interleukins, and tumor necrosis factor are also released, which trigger the gradual destruction of the articular cartilage over time.
Natural History
Glenohumeral arthritis leads to progressive stiffness, pain, and loss of function of the shoulder. Full thickness rotator cuff tears only occur in 5% to 10% of the patients with primary arthritis. Rheumatoid arthritis results in progressive regional osteopenia, central glenoid bone erosion, and rotator cuff tears. Full thickness rotator cuff tears in RA occur in 25% to 40% of the patients, but rotator cuff dysfunction and tearing are very common.
Clinical Presentation
A patient with shoulder arthritis typically presents with severe, escalating shoulder pain, loss of range of motion (primarily external rotation of the shoulder), difficulty sleeping, and loss of shoulder function. Physical examination will focus on the integrity and function of the rotator cuff, which is important to consider when deciding on the appropriate treatment approach.
Differential Diagnosis
- Frozen shoulder
- Posttraumatic or post-surgical infection
- Cervical stenosis
- Cervical radiculopathy
- Neoplasm
Nonoperative Management
- Avoid activities that exacerbate the pain such as weight lifting or overhead activities (activity modification).
- NSAIDs (Non-steroidal anti-inflammatories)
- Intra-articular injections:
- Corticosteroid injections
- Hyaluronic Acid (not yet approved by the FDA)
- Platelet-rich plasma or BMAC injections
- Physical therapy
Surgical Management
Surgical options for the management of advanced glenohumeral arthritis include:
- Total shoulder arthroplasty/replacement (TSA)
- Hemiarthroplasty
- Reverse shoulder arthroplasty (RSA)
- Arthroscopic debridement
- Arthrodesis
The primary indications for a total shoulder arthroplasty (TSA) include the failure of an extensive course of non-operative management with an intact rotator cuff in the context of advanced osteoarthritis. In comparison, the primary indication for a reverse shoulder arthroplasty (RSA) is an irreparable rotator cuff tear in the context of advanced osteoarthritis.
If you are suffering from shoulder pain or arthritis, contact Dr. Dold for a consultation today!
Clinical Studies
- Biologic Options for Glenohumeral Arthritis. Clin Sports Med 2018.
- Glenohumeral Osteoarthritis in the Young Patient. JAAOS 2018.
- Surgical options for the young patient with glenohumeral arthritis. Int J Shoulder Surg 2016.
- Biologic resurfacing arthroplasty with acellular human dermal allograft and platelet-rich plasma (PRP) in young patients with glenohumeral arthritis-average of 60 months of at mid-term follow-up. J Shoulder Elbow Surg 2016.
- Arthroscopic Management of Glenohumeral Arthritis: A Joint Preservation Approach. JAAOS 2018.
- Nonarthroplasty Options for the Athlete or Active Individual with Shoulder Osteoarthritis. Clin Sports Med 2018.
- Survivorship and Patient-Reported Outcomes After Comprehensive Arthroscopic Management of Glenohumeral Osteoarthritis: Minimum 5-Year Follow-up. Am J Sports Med 2016.
- Comprehensive Arthroscopic Management of Glenohumeral Osteoarthritis: Preoperative Factors Predictive of Treatment Failure. Am J Sports Med 2017.
- Predictors for satisfaction after anatomic total shoulder arthroplasty for idiopathic glenohumeral osteoarthritis. Arch Orthop Trauma Surg 2016.
- High Satisfaction and Return to Sports After Total Shoulder Arthroplasty in Patients Aged 55 Years and Younger. Am J Sports Med 2017.
- Patient Activity Levels After Reverse Total Shoulder Arthroplasty: What Are Patients Doing? Am J Sports Med 2015.
- Return to sport after shoulder arthroplasty: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 2018.
- Return to Play After Shoulder Replacement Surgery: What Is Realistic and What Does the Evidence Tell Us. Clin Sports Med. 2018.
- A comparative analysis of work-related outcomes after humeral hemiarthroplasty and reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017.
- Functional outcome of hemiarthroplasty compared with reverse total shoulder arthroplasty in the treatment of rotator cuff tear arthropathy. J Shoulder Elbow Surg. 2012.
- Clinical outcomes of reverse total shoulder arthroplasty in patients aged younger than 60 years. J Shoulder Elbow Surg. 2014.
- Rate of Improvement in Clinical Outcomes with Anatomic and Reverse Total Shoulder Arthroplasty. J Bone Joint Surg Am. 2017.
- How reverse shoulder arthroplasty works. Clin Orthop Relat Res. 2011.
- Comparison of liposomal bupivacaine infiltration versus interscalene nerve block for pain control in total shoulder arthroplasty: A meta-analysis of randomized control trials. Medicine (Baltimore). 2017.
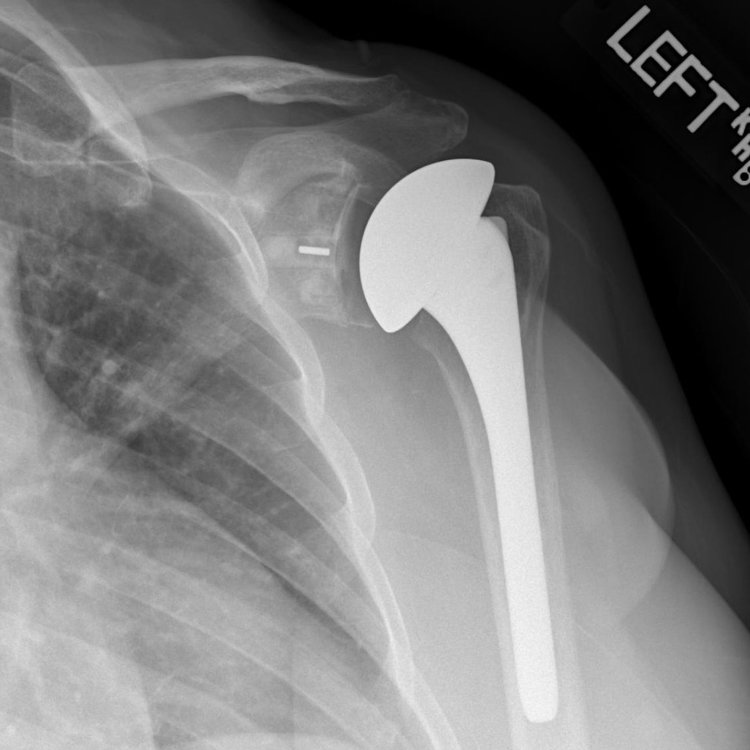
Xray of the left shoulder following total shoulder arthroplasty (TSA).


