Anatomy:
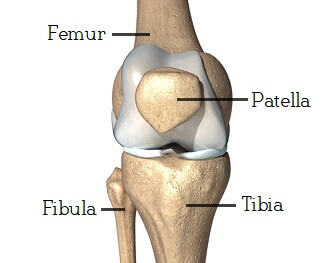
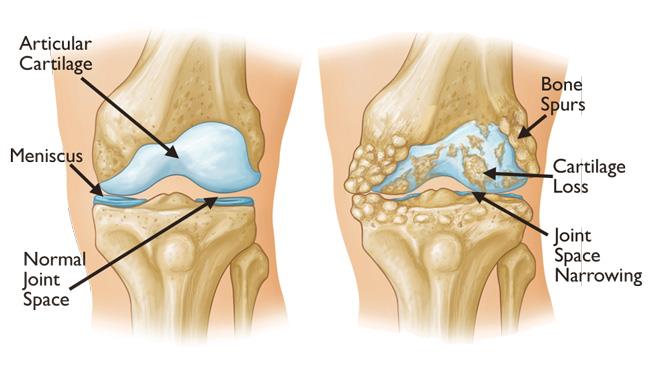
The knee joint is a classic hinge joint that is created by the articulation of the femur (thigh bone), tibia (shin bone), and patella (kneecap). There are three compartments, or individual joints, that create the knee joint: medial, lateral, and the patellofemoral joint. When all three compartments are affected by arthritis, we term this “tricompartmental osteoarthritis.” This knee is one of the largest and most complex joints in the body. Ligaments, tendons, muscle, and menisci help provide stability and hold the joint together. The articular surfaces of the joint are coated in hyaline cartilage, which provides a smooth surface for the knee to glide and move freely through its range of motion arc. Arthritis simply refers to the loss of the normal articular cartilage of a joint and the inflammatory cascade and symptoms that develop along with this process. Below the hyaline cartilage lies subchondral bone (sub = below; chondral = cartilage). This subchondral bone is what becomes exposed in the advanced stages of osteoarthritis, which is commonly referred to as “bone on bone arthritis.” The surgical treatment of end-stage, tricompartmental knee arthritis is a total knee arthroplasty/replacement (TKA).
Etiology:
Osteoarthritis of the knee is thought to be the result of multiple risk factors that ultimately lead to the degeneration of hyaline cartilage along the articular surfaces of the knee. These risk factors can be modifiable and non-modifiable.
Modifiable risk factors include:
- Weight/BMI
- Activity level – A decrease in activity level can lead to reduced cell turnover and ultimately degeneration in cartilage. A regular exercise regimen will help protect the joint and reduce stress while also helping maintain a normal BMI
- Occupation – some occupations that require increased time in a squatting or kneeling position can lead to excess unwanted stress across the knee joint.
- Muscle weakness
- Metabolic syndrome
- Joint trauma/injury
Non-modifiable risk factors include:
- Increased age – Natural age-related changes lead to decrease in hyaline cartilage associated with OA. Unfortunately, this is the most well known risk factor associated with OA.
- Gender – Women have a higher chance of developing OA than men at a 2:1
- Genetics – Recent studies have shown a larger genetic influence on the development of OA than previously thought.
- Prior injury or periarticular fracture
- Race
- Previous knee joint infection (septic arthritis)
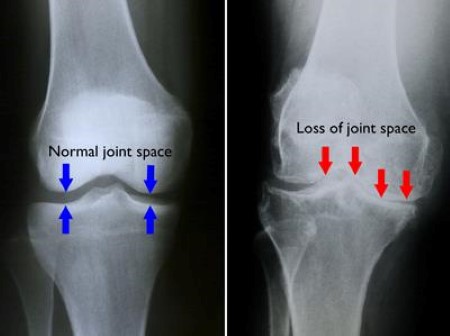
Diagnosis:
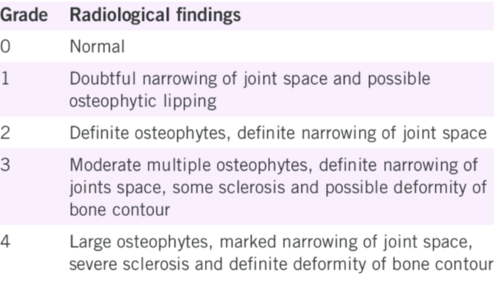
The diagnosis of knee osteoarthritis can be made clinically with a series of radiographs obtained in our office. Plain film radiographs show the joint space within the knee and can be used to help classify the extent of arthritis on a scale of 0 to 4.
Treatment:
The treatment of knee osteoarthritis typically begins with conservative, non-operative measures and gradually moves up the treatment ladder to include more invasive interventions as the disease progresses. Typically, we would like to preserve the most invasive option (Total Knee Arthroplasty) for a last resort when all other treatment options have failed.
- Non-operative treatment options:
- Weight reduction – For patients with an elevated BMI (> 25), weight reduction is the single most important modifiable risk factor for symptomatic arthritis. We suggest weight loss for patients with symptomatic osteoarthritis of the knee and a BMI ≥ 25. BMI is Body Mass Index. Normal body weight is defined as a BMI between 18.5 and 25. The clinical definition of obesity is a BMI > 30. Studies show that each pound of weight lost will result in a 4-fold reduction in the load exerted on the knee per step during daily activities (ex. For people losing 10 pounds, each knee would be subjected to 48,000 pounds less in compressive load per mile walked). What is your BMI? If it is greater than 25, you will significantly benefit from weight loss.
- Physical therapy and exercise – We recommend that patients with symptomatic osteoarthritis of the knee participate in self management programs, strengthening, low-impact aerobic exercises, and neuromuscular education; and engage in physical activity consistent with national guidelines.
- Oral Glucosamine and Chondroitin Sulfate Supplements – Although the literature is mixed, various studies have shown an improvement in knee symptoms in patients taking these over-the-counter supplements.
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) or Tramodol – A large body of evidence exits to support the use of NSAIDs for symptomatic improvement in patients suffering from arthritis. Ex. Meloxicam, Celebrex, Aleve, Ibuprofen, Naproxen, etc.
- Bracing – Osteoarthritis of the knee often involves and affects one compartment of the knee more so than the others (Remember: There are 3 compartments that make up the knee joint; typically, one compartment is affected more than the others). Occasionally, arthritis only affects one compartment while completely sparring the others. In these cases, offloading the primarily affected compartment can greatly relieve a patient’s symptoms. An offloader brace can be prescribed to change the angle and weight distribution across the knee, reducing the load on the affected compartment to decrease pain. Many patients report that wearing the brace during exercise and activity can really help! Furthermore, studies have shown that reducing load across an arthritic joint can even help regenerate cartilage and halt the arthritic process!
- Injections – Various injections have been studied for the management of osteoarthritis. Dr. Dold has published his research on these various therapies, including PRP, BMAC, and stem cell alternatives, in various peer-reviewed journals: Dold, A et al. Injectable Biological Treatments for Osteoarthritis of the Knee. JBJS Reviews, 2017.
- Corticosteroid (“Cortisone”): A corticosteroid mimics the action of naturally occurring hormones secreted by your adrenal glands. When delivered in doses that exceed your body’s natural levels, a corticosteroid functions as a potent anti-inflammatory, supressing your body’s natural inflammatory response. As a result, the inflammation and pain associated with arthritis is inhibited/decreased. While the effect is immediate, the response may only last up to 3 months and is associated with various side effects, including infection. Overuse of corticosteroid can also have a catabolic effect, causing cartilage to breakdown and deteriorate further, exacerbating the symptoms of arthritis over time.
- Hyaluronic Acid (aka. “Gel Injections / “Viscosupplementation” / “Synvisc”): Joints are like gears – they work best if they’re well lubricated. In a healthy joint, a thick substance called synovial fluid provides lubrication, allowing bones to glide against one another. Synovial fluid acts as a shock absorber, too. In people with osteoarthritis, a critical substance in synovial fluid known as hyaluronic acid breaks down. Loss of hyaluronic acid appears to contribute to joint pain and stiffness. Many studies have shown a significant improvement in patient symptoms following a course of hyaluronic acid injections. These injections are occasionally covered by insurance every 6 months. Ex. Durolane, GelSyn, TriVisc, GelOne, Synvisc, etc.
- Platelet-Rich Plasma (PRP): The use of PRP for knee arthritis has been studied extensively, and the results are promising. In fact, PRP has outperformed both cortisone and hyaluronic acid in long-term follow-up trials and meta-analyses. Unlike cortisone, PRP is not associated with any adverse outcomes while helping to nourish, protect, and prevent further cartilage breakdown within the joint. The procedure takes roughly 30 minutes. Approximately 30mL of your whole blood is drawn and placed in a centrifuge to spin for 15 minutes. The centrifugal force allows us to separate and isolate the platelets, formulating a platelet-rich product that is then injected back into your knee joint. PRP is a rich source of growth factors that stimulate healing and regeneration of damaged tissue, while serving as a potent, natural anti-inflammatory. Since the product is derived from your own body, there is no risk of “rejection.” Unfortunately, PRP is not covered by private insurance or Medicare – it is still considered an “experimental” therapy. We recommend a series of 3 injections, one week apart over 3 weeks: PRP/PRP/PRP or BMAC/PRP/PRP. *Recently, Hyaluronic Acid in combination with PRP has shown even better results than either treatment used alone. Consider a series of three HA + PRP injections.
- Mesenchymal Stem Cell (MSC) Therapy (Bone Marrow Aspirate Concentrate – “BMAC”) – Bone marrow is one of the primary sources of stem cells in our bodies. In a BMAC procedure, bone marrow is aspirated from the iliac crest of the pelvis and then centrifuged (similar to PRP) in order to separate out the mesenchymal stem cells (MSCs). These cells are then isolated and injected back into the knee joint. The procedure is performed in office under local anesthetic with minimal discomfort. MSCs have regenerative potential but also serve as the richest source of growth factors and anti-inflammatory cytokines within the body. In addition to providing a potent stimulus for growth and healing (a paracrine effect), the regenerative stem cells (“materials”) are also delivered directly into the affected joint to promote an anabolic effect with the potential to regenerate tissue. Unfortunately, BMAC is not covered by private insurance or Medicare.
- Amniotic Fluid Therapy (“Amnio”) or Placental/Umbilical Cord Tissue Therapy – Recently, amniotic fluid and tissue has generated interest and fascination among clinicians and patients as a potential source of prefabricated “stem cells” (ie. ‘Stem cells in a vial’). While amniotic tissues provide a rich source of growth factors (similar to PRP), the commercially available products cannot be considered a true source of stem cells (pluripotent cells). However, their clinical application and benefit is under constant review with new studies appearing regularly in the literature. Unfortunately, amniotic and umbilical products are typically not covered by private insurance or Medicare. In certain situations with certain payors, we are able to get these products covered by insurances; however, this is typically not the case.
Operative Treatment:
The surgical treatment for end-stage osteoarthritis of the knee is a Total Knee Arthroplasty (TKA), also known as a knee replacement. Once ALL conservative management options have been considered, we would consider a TKA as the next, and final, option for the management of knee arthritis. TKA is the gold standard for treating end stage osteoarthritis of the knee. This procedure can lead to a reduction in symptoms and an increase in the quality of life for anyone suffering from symptomatic knee arthritis that has failed conservative management options.
Dr. Dold performs hundreds of knee replacements every year. To schedule a consultation with Dr. Dold, click HERE. Our team will be in contact with you within 24 hours of receiving your request online (typically within an hour).
Related articles:
- NEJM: Osteoarthritis of the Knee. 2021.
- JAAOS: Management of osteoarthritis of the knee in the active patient. 2010.
- JAAOS: Degenerative arthritis of the knee in active patients: evaluation and management. 1999.
- KSSTA: Radiological grading of osteoarthritis on Rosenberg view has a significant correlation with clinical outcomes after medial open-wedge high-tibial osteotomy. 2019.
- J Knee Surg: Unicompartmental Knee Arthroplasty: The Past, Current Controversies, and Future Perspectives. 2018.
- J Arthroplasty: Unicompartmental Knee Arthroplasty vs Total Knee Arthroplasty for Medial Compartment Arthritis in Patients Older Than 75 Years: Comparable Reoperation, Revision, and Complication Rates. 2017.


