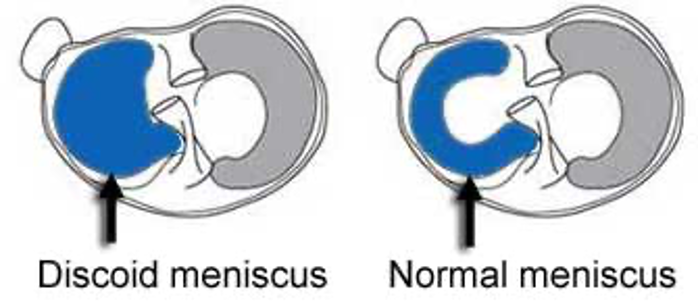
The knee joint (tibiofemoral joint) contains two c-shaped menisci: medial and lateral. Menisci are crucial to knee function and joint health. These structures help to stabilize the knee while optimizing force transmission. A discoid meniscus is an abnormal meniscus based on meniscus morphology. A discoid meniscus is characterized by its disc or oval shape and abnormally thick cartilage. Due to the abnormal shape of a discoid meniscus, this structure is more prone to injuries compared to a regular c-shaped meniscus. The lateral meniscus is most commonly affected. A discoid meniscus causes increase in mobility of the meniscus which may result in a meniscal tear. Meniscal tears can be addressed either with partial meniscectomy or meniscal repair. In the setting of discoid meniscus, saucerization of the meniscus may be performed. This involves re-shaping the meniscus to a normal shape while removing any torn meniscal fragments in the process. The aim is to restore normal meniscal architecture and function while preserving as much of the meniscal tissue as possible.
Anatomy
The menisci help to distribute loads and stresses on the knee joint. They are made of fibroelastic cartilage. 90% of the collagen they are composed of is Type 1 collagen. The lateral meniscus is useful with posterior movement while the medial meniscus is involved in preventing anterior translation with knee extension. In an ACL deficient knee, the menisci become imperative stabilizers of the tibiofemoral joint. To optimize force transmission, the menisci increase contact surface area and absorb shock using their radial and longitudinal fibers. The abnormal shape of the discoid meniscus makes a patient more susceptible to meniscal tearing. Discoid menisci can be divided into 3 categories: incomplete, complete, and hypermobile Wrisberg variant.
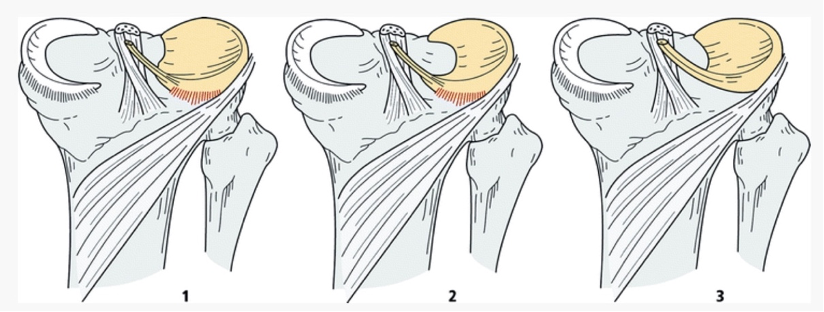
An incomplete discoid meniscus or type 1 is block-shaped, covers the entire tibial plateau, and has a normal posterior attachment making it stable. Type 2 or incomplete discoid meniscus does not span the entire tibial plateau, though it is also stable with normal posterior attachment. Type 3 or Wrisberg-type has similar appearance to a regular c-shaped meniscus, but does not have posterior attachment and is only attached by the Wrisberg ligament to the posterior horn of the lateral meniscus. This type is the least stable of the three.
Pathogenesis
A discoid meniscus is a congenital defect without known cause though likely due to failure of apoptosis in utero. The lateral meniscus is the most commonly affected. 1 in 4 discoid menisci are located in bilateral knees. Discoid meniscus affects approximately 5% of the population and is often found in adolescents and young adults.
Presentation
Discoid meniscus can be asymptomatic. Patients may present with pain, swelling, mechanical locking or catching of the knee when in knee extension, clicking, or difficulty with knee extension. These are referred to as “mechanical symptoms.” Symptoms for this condition may not develop until adolescence.
Patients may experience clicking and popping in the knee during range of motion testing. Pain can be made worse with knee extension. There can also be tenderness located along the lateral meniscus. Pain within a discoid meniscus is likely due to a disruption in one or both of the menisci which causes pain and swelling in the knee especially with activity. Injury to a discoid meniscus is often related to a twisting or pivoting type injury. The injury often occurs during a sport such as tennis, soccer or basketball.
Imaging
Imaging is often used to confirm the diagnosis of a discoid meniscus. On X-rays, there may be squaring of the lateral condyle, cupping of the lateral tibial plateau, and widening of the joint space.
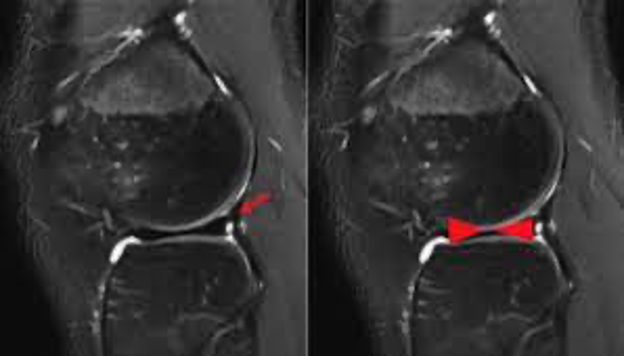
MRI assists in further characterizing the morphology of the meniscus and to determine if there are any tears or disruptions within the meniscus. “Bow-tie sign” can be found on MRI which demonstrates meniscal continuity on >3 sagittal images. Differential diagnosis include: osteoarthritis of the knee, patellar femoral syndrome, IT band syndrome, tibial stress fracture, lumbar spine pathology, bone contusion, knee sprain, plica syndrome, meniscal tear, and osteochondral lesion.
Treatment options
Do nothing! A discoid meniscus can be an incidental finding. Patients may go their whole life without pain or symptoms. In cases where patients are symptomatic, a knee arthroscopy with partial meniscectomy and saucerization can be performed. Saucerization involves cutting the abnormally thick discoid meniscus and reshaping the meniscus to a more normal morphology. Meniscal tears are the most common indication for knee surgery. Surgical intervention for an isolated meniscus tear is often completed as a knee arthroscopy to address the defect using a camera for visualization of the knee joint. A knee scope may involve a meniscectomy, cutting out the small portion of torn meniscus, or a meniscal repair. In the setting of a Wrisberg variant, a meniscal repair is often indicated. Meniscal repair can be achieved utilizing suture and anchors. Meniscal repair techniques include: inside out, all inside, outside in, and open repair. Tears located in the white zone, with little to no blood supply, are often treated with a partial meniscectomy. If the meniscus tear or tears are present in the setting of significant osteoarthritis, the knee may be need to be replaced and a total knee arthroplasty is performed. Recovery time depends on the procedure performed. Meniscus repair requires adequate time for healing of the repaired tissue and typically takes approximately 6 months to heal. Patient’s undergoing meniscal repairs are often six weeks non-weight bearing utilizing crutches and a brace. Partial meniscectomy patients typically do not require crutches and bracing for greater than a week.
To set up a knee consultation with Dr. Dold click HERE.
YouTube of Dr. Dold’s arthroscopic partial meniscectomy can be viewed HERE.
YouTube of Dr. Dold’s arthroscopic partial meniscal root repair can be viewed HERE.
Related Research
- Discoid Meniscus.
- Discoid meniscus: current concepts.
- Discoid Lateral Meniscus.
- Symptomatic Discoid Meniscus in Children and Adolescents: A Review of 470 Cases.
- Discoid meniscus in human fetuses: A systematic review.
- Discoid lateral meniscus.
- Discoid meniscus.
- Update on imaging of the discoid meniscus.
- Discoid lateral meniscus: current concepts.
- Discoid Lateral Meniscus in Children: Diagnosis, Management, and Outcomes.
- Discoid Meniscus: Diagnosis and Management.
- Discoid medial meniscus.
- Symptomatic Complete Discoid Medial Meniscus Completely Coalesced with the Anterior Cruciate Ligament: A Case Report and Literature Review.
- Discoid Meniscus in the Pediatric Population:: Emphasis on MR Imaging Signs of Instability.
- The Natural History of Meniscus Tears.
- Partial resection of lateral discoid meniscus changes lower limb axial alignment – A retrospective cohort study.
- Diagnosis and Treatment of Discoid Meniscus.
- Review of discoid meniscus.
- Histological Study of Discoid Lateral Meniscus in Children and Adolescents: Morphogenetic Considerations.
- Discoid medial meniscus of both knees: A case report.
- Discoid lateral meniscus in children.
- Pediatric discoid meniscus: can magnetic resonance imaging features coupled with clinical symptoms predict the need for surgery?