Overview and Anatomy:
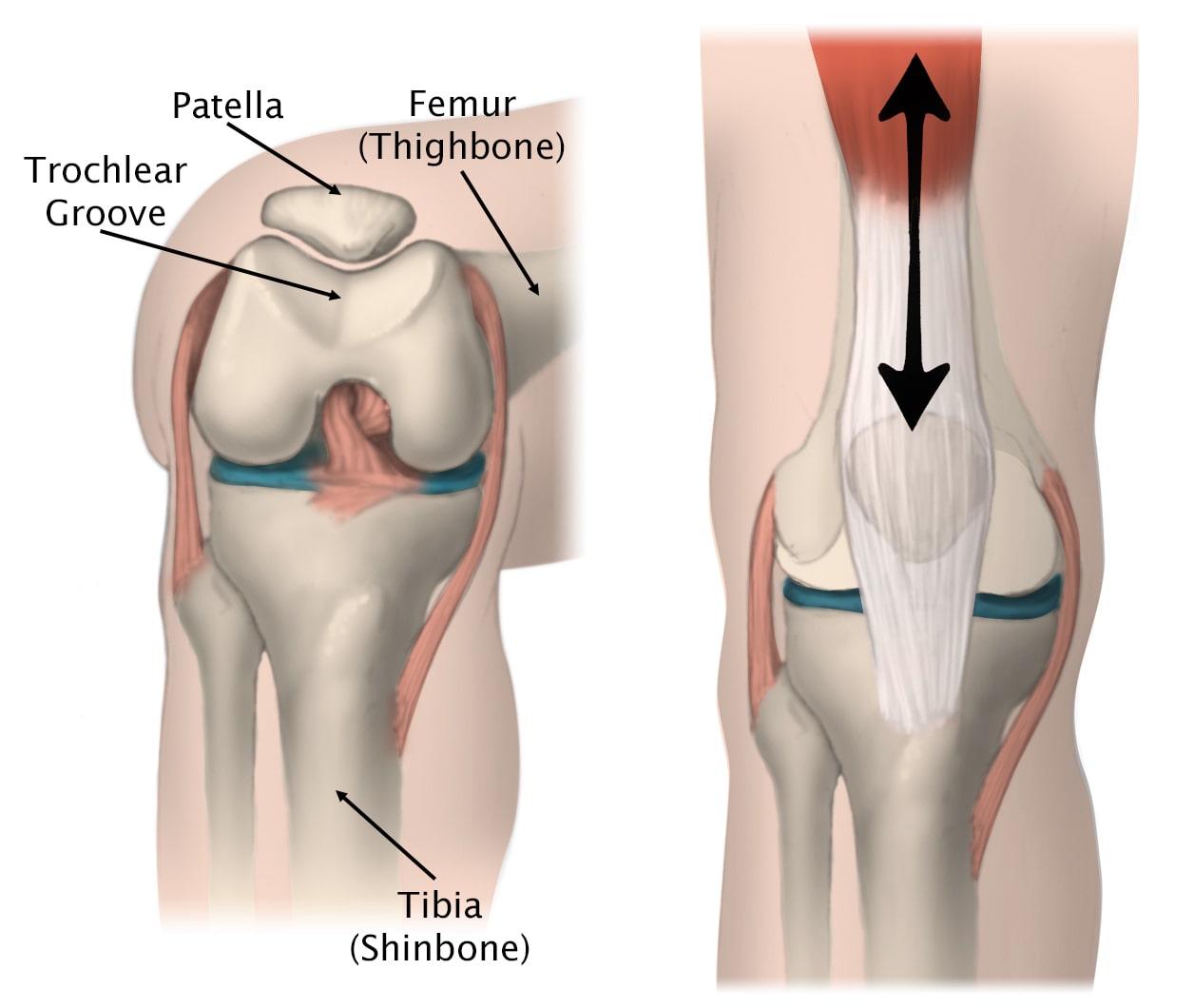
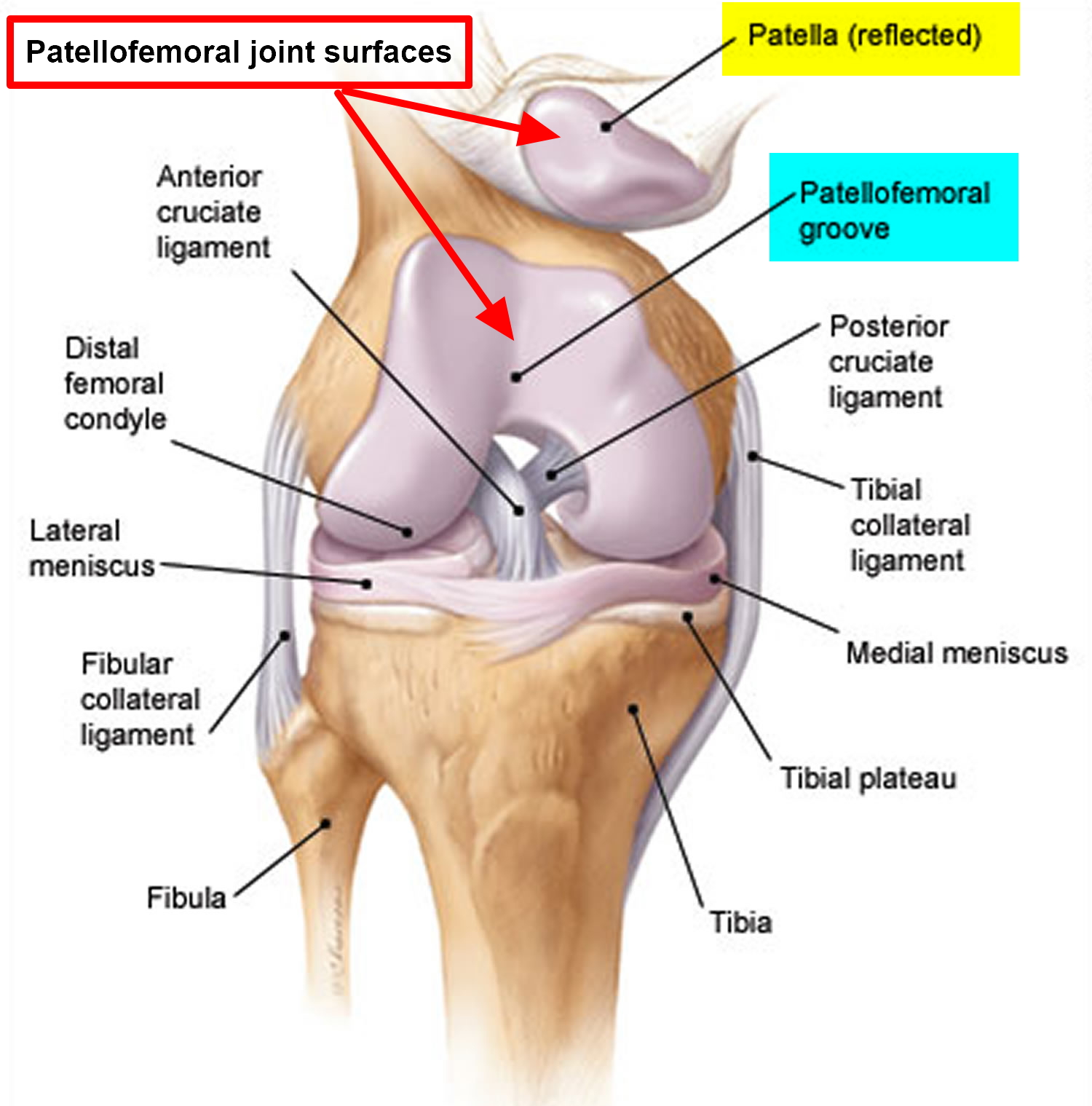
Patellofemoral Syndrome, also referred to as Anterior Knee Pain or Runner’s Knee, is a condition affecting the articulation/joint between the back of the patella (knee cap) and the front of the distal femur (thigh bone or trochlea). The patella sits in a shallow groove in the front of the femur known as the trochlear groove. Together, the patella and the trochlear groove make up the patellofemoral joint (PFJ) of the knee. Inflammation and resulting pain of the patellofemoral joint is referred to as Patellofemoral Joint Syndrome, also known as PFJ syndrome, anterior knee pain, or runner’s knee. The patella glides up and down the trochlear groove during motion of the knee. Patients typically complain of pain in the front (or ‘anterior’ aspect) of their knee that is worse with flexion or specific exercises that involve flexion/extension of the knee (ex. Walking up/down stairs, rising from a seated position, running, lunging, squatting, etc). Increasing quadriceps muscle strength will help to offload the patellofemoral joint and improve the symptoms associated with PFJ syndrome. Focusing on vastus medialis oblique (VMO) muscle strength and proprioception will help to improve patellofemoral joint tracking and improve symptoms associated with PFJ syndrome.
Etiology:
The underlying cause of patellofemoral syndrome is increased pressure within the patellofemoral joint, due to maltracking of the patella, which ultimately leads to inflammation and pain within the joint. This is most commonly due to an imbalance of the muscles that control and stabilize the patella within the trochlear groove. For example, when the hamstrings overpower the quads (or are stiff or tight relative to the quads), pressure within the PF joint increases and can cause pain over time. In this case, the treatment is simple: Strengthen the quads and stretch the hamstrings!
Causes of increased pressure within the PF joint include:
- Quadriceps muscle imbalance or relative weakness in comparison to the hamstrings (Hamstrings > Quads)
- Tight hamstrings
- Malalignment or maltracking of the patella as it moves through the trochlear groove (resulting from muscle imbalance around the knee)
- Excessive sitting (leading to tight hamstrings and relative weakness of the quadriceps)
- Prolonged or repetitive compression or shearing forces within the PF joint (ex. Running, jumping, squatting, etc)
Diagnosis:
History
A patient’s pain is commonly located in the front of the knee (peripatellar or anterior knee pain). Pain can occur a with sudden increase in activity such as starting a new workout plan or a runner upping their mileage. Pain is often exacerbated by walking up and down stairs, prolonged sitting, squatting, and kneeling. Patient may notice a creaking sound in their knee called crepitus.
Physical Exam
On physical exam, there may be crepitus, patellar maltracking, and quadricep muscle weakness (underdeveloped quads muscles or a relative weakness of the quads compared to the hamstrings). There may be swelling or an effusion present. Patellar grind test or Clark’s compression test is often positive: the patient is placed in the supine position with the knee extended. Pressure is applied just superior to the patella with the examiner’s hand. The patient then gradually contracts and releases their quadricep muscle. If this contraction elicits pain, the test is positive. The examiner will also assess the patient’s Q-angle, a measurement of the angle between the quadriceps muscles and the patella tendon. Q-angle is considered clinically as a very important parameter which displays the biomechanical effect of the quadriceps muscle on the knee, and it is also regarded a crucial factor for the proper posture and movement of the patella. The Q angle is routinely and regularly used as an assessment parameter during the diagnosis of many knee-related problems, including anterior knee pain, osteoarthritis, and degenerative knee disorders.
Imaging:
X-rays may show chondrosis, lateral patella tilt, or a shallow trochlear groove (trochlear dysplasia). Chondrosis is cartilage breakdown in the knee. Lateral patella tilt indicates that the patella is improperly tracking. A shallow sulcus can indicate patellar instability caused by dysplasia. Trochlear dysplasia refers to a pathologic alteration in the shape of the femoral trochlea. Whereas a normal trochlea (also known as facies patellaris, intercondylar groove, or intercondylar sulcus) is sufficiently concave to guide and retain the patella throughout the normal range of arc, a dysplastic trochlea may be shallower than normal or even flat or convex, predisposing the patella to lateral subluxation or even dislocation. This is known as patella instability.
MRI is the image of choice to visualize abnormal patellar cartilage, though is often unnecessary for diagnosis of PFJ syndrome.
Treatment:
Patellofemoral Syndrome is most commonly treated by conservative measures. These include:
- Physical Therapy (Stretching, Strengthening, Proprioception)
- Patella-stabilizing knee brace or taping (ex. U- or J-brace)
- NSAIDs to relieve inflammation within the joint
- Icing
- Injections (Corticosteroid or Platelet-rich plasma/PRP)
The most important aspect to therapy is aggressive quadriceps strengthening (focusing on vastus medialis oblique, VMO) and stretching of the quads and hamstrings to help relieve the muscle imbalance responsible for the increased pressure and maltracking of the patella across the knee. Occasionally, inflammation within the joint can be treated with intra-articular injections of corticosteroids, platelet-rich plasma (PRP), or stem cells. Dr. Dold can discuss these options with you.
Physical Therapy:
This rehabilitation protocol is intended for patients suffering from patellofemoral syndrome. Rehab should focus on the following
- Stretching and Strengthening of the following muscle groups:
- Quadriceps (strengthening of VMO)
- Hamstrings
- Adductors
- ITB
- Hip Flexors
- Gastrocnemius/Soleus
- Proprioception
- Dynamic stabilizing exercises of the patellofemoral joint
- Taping to improve patellar tracking +/- bracing
- Modalities to reduce swelling and inflammation and treat atrophy, including:
- Electrical muscle stimulation
- Ultrasound
- Transcutaneous Nerve Stimulation (TENS)
- Ice/Cold Packs
A particular focus should be placed on aggressive quads strengthening and stretching of the quads and hamstrings!
Particular focus on VMO strengthening: YouTube.com → “vmo strengthening exercises” – this needs to become part of your daily routine.
Goals of therapy:
- Improve strength and flexibility of the lower extremity musculature, with a primary focus on the quads, hamstrings, and glutes.
- Decrease pain, swelling, and atrophy utilizing available modalities
- Increase range of motion and overall lower extremity joint mobility
- Initiate a home exercise program → focus on VMO strengthening routine (daily)
- Educate patient on pathophysiology of the disorder (the biomechanics of patella maltracking)
- Educate patient on taping techniques and/or brace application
Overall, a pain-free return to sport should be achieved within 4-6 weeks of dedicated physical therapy! It is important to note that recovery and return-to-play is largely “patient dependent.” If YOU put in the work and focus on your rehab to improve your strength and flexibility, your pain WILL improve!! Stay dedicated to your rehab plan and recovery!
Dr. Dold specializes in the management of all knee conditions including management of patellofemoral syndrome. To schedule a new patient consultation, please fill out a form and a member of our team will reach out to you within 24 hours to confirm your appointment.
To view Dr. Dold’s Video on the importance of physical therapy click here:
Related Articles and Research on PFJ Syndrome:
- Patellofemoral pain syndrome.
- Patellofemoral Pain Syndrome.
- Effectiveness of conservative treatment for patellofemoral pain syndrome: A systematic review and meta-analysis.
- Systematic Review of the Effect of Taping Techniques on Patellofemoral Pain Syndrome.
- Management of patellofemoral pain syndrome.
- Osteopathic Manipulative Treatment Versus Exercise Program in Runners With Patellofemoral Pain Syndrome: A Randomized Controlled Trial.
- Current clinical, radiological and treatment perspectives of patellofemoral pain syndrome.
- Factors associated with patellofemoral pain syndrome: a systematic review.
- Effectiveness of hip muscle strengthening in patellofemoral pain syndrome patients: a systematic review.
- Patellofemoral Pain.
- Study protocol: a randomised controlled trial comparing the long term effects of isolated hip strengthening, quadriceps-based training and free physical activity for patellofemoral pain syndrome (anterior knee pain).
- Clinical test for diagnosis of patellofemoral pain syndrome: Systematic review with meta-analysis.
- Comparison of mobilization with movement and Mulligan knee taping on Patellofemoral pain syndrome.
- Patellofemoral pain: epidemiology, pathophysiology, and treatment options.
- The effects of additional kinesio taping over exercise in the treatment of patellofemoral pain syndrome.
- Effectiveness of local exercise therapy versus spinal manual therapy in patients with patellofemoral pain syndrome: medium term follow-up results of a randomized controlled trial.
- Effects of neuromuscular training on pain intensity and self-reported functionality for patellofemoral pain syndrome in runners: study protocol for a randomized controlled clinical trial.
- Effects of tibiofemoral mobilization in patients of Patellofemoral pain syndrome.
- Effects of Static and Dynamic Stretching With Strengthening Exercises in Patients With Patellofemoral Pain Who Have Inflexible Hamstrings: A Randomized Controlled Trial.
- Patellofemoral Pain Syndrome Risk Associated with Squats: A Systematic Review.
- Risk factors for patellofemoral pain: a systematic review and meta-analysis.
- Is hip strengthening the best treatment option for females with patellofemoral pain? A randomized controlled trial of three different types of exercises.
- A Systematic Review of Clinical Practice Guidelines for Physical Therapist Management of Patellofemoral Pain.
- The Effect of Kinesio Taping on Anterior Knee Pain Consistent With Patellofemoral Pain Syndrome: A Critically Appraised Topic.
- Neuromuscular training and muscle strengthening in patients with patellofemoral pain syndrome: a protocol of randomized controlled trial.
- Hip and Knee Strengthening Is More Effective Than Knee Strengthening Alone for Reducing Pain and Improving Activity in Individuals With Patellofemoral Pain: A Systematic Review With Meta-analysis.
- Patellofemoral pain: One year results of a randomized trial comparing hip exercise, knee exercise, or free activity.


