Dr. Dold has published the first review of posteromedial corner injuries:
The Posteromedial Corner of the Knee: Anatomy, Pathology, and Management Strategies
Dold, Andrew P. et al. JAAOS: 2017 Nov; 25(11):752-761.
Abstract
The posteromedial corner of the knee encompasses five medial structures posterior to the medial collateral ligament. With modern magnetic resonance imaging systems, these structures are readily identified and can be appreciated in the context of multiligament knee injury. It is recognized that anteromedial rotatory instability results from an injury that includes both the medial collateral ligament and the posterior oblique ligament. Like posterolateral corner injuries, untreated or concurrent posteromedial corner injuries resulting in rotatory instability place additional strain on anterior and posterior cruciate ligament reconstructions, which can ultimately contribute to graft failure and poor clinical outcomes. Various options exist for posteromedial corner reconstruction, with early results indicating that anatomic reconstruction can restore valgus stability and improve patient function.
Introduction
The lateral side of the knee has historically been considered the “dark side of the knee” owing primarily to our previous lack of knowledge of both the complex anatomy in this region and the management of posterolateral corner (PLC) pathology. Extensive research has since focused on the evaluation and management of PLC injuries, which has resulted in a simplified approach and improved understanding of this area of the knee.2 Considerably less literature has focused on the medial side of the knee, specifically, the posteromedial corner (PMC), with some authors labelling it “the neglected corner.”3 This may be due to the initial research and subsequent functional studies, which focused predominantly on the role of the superficial medial collateral ligament (MCL), with little emphasis on the supporting posteromedial structures.4 As a result, medial-sided knee injury has become synonymous with injury to the superficial MCL,5 with a lack of appreciation and understanding of the other structures involved.
With modern magnetic resonance imaging systems, the major anatomic structures comprising the PMC can be readily identified. Recent anatomic and biomechanical studies have expanded our understanding of these medial structures and their contribution to the static and dynamic stability of the knee, including their supporting role in multiligament knee injuries. It is recognized that anteromedial rotatory instability (AMRI) results from an injury that includes both the medial collateral ligament (MCL) and the posterior oblique ligament (POL). Like PLC injuries, untreated or concurrent PMC injuries resulting in rotatory instability place additional strain on ACL and PCL reconstructions, which can ultimately contribute to graft failure and poor clinical outcomes.
Anatomy
The anatomy of the medial side of the knee has been described by two different approaches. Initially, Warren et al4 divided the medial side into three layers from superficial to deep. Layer I consisted of the deep fascia, layer II consisted of the superficial Medial Collateral Ligament (MCL), and layer III consisted of the joint capsule and the deep MCL. Little attention was given to the structures lying posterior to the MCL in this “layered approach.”
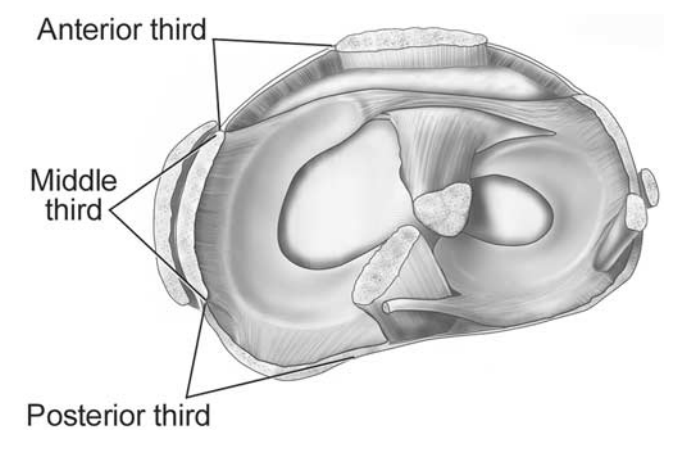
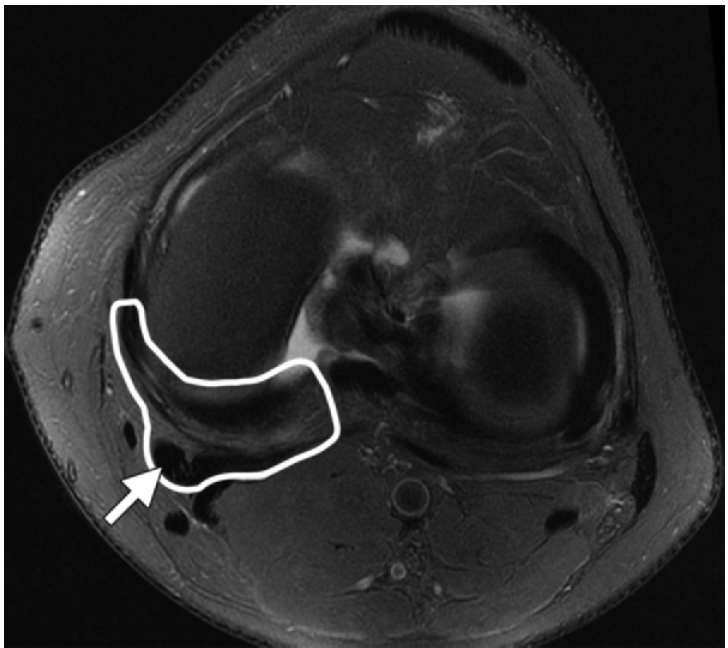
A more recent description by Robinson et al6 divided the medial side of the knee into thirds – anterior, middle, and posterior – extending circumferentially from the medial edge of the patellar tendon anteriorly to the most medial edge of the medial head of gastrocnemius posteriorly. The anterior third extends from the medial border of the patellar tendon to the anterior border of the longitudinal fibers of the superficial MCL. The middle third is comprised of the width of the longitudinal fibers of the MCL. The posterior third, encompassing the PMC of the knee, extends from the posterior border of the longitudinal fibers of the superficial MCL to the medial edge of the medial head of gastrocnemius, which lies adjacent to the medial margin of the posterior cruciate ligament (PCL). (Figure 1).
Components of the Posteromedial Corner
There are five major components that make up the PMC of the knee: the posterior oblique ligament (POL), the semimembranosus tendon and its expansions, the oblique popliteal ligament (OPL), the posteromedial joint capsule, and the posterior horn of the medial meniscus. The superficial and deep portions of the MCL occupy the middle third of the medial side of the knee and, although they function in close association with the structures of the PMC, are not typically considered part of the PMC.3
Posterior Oblique Ligament (POL)
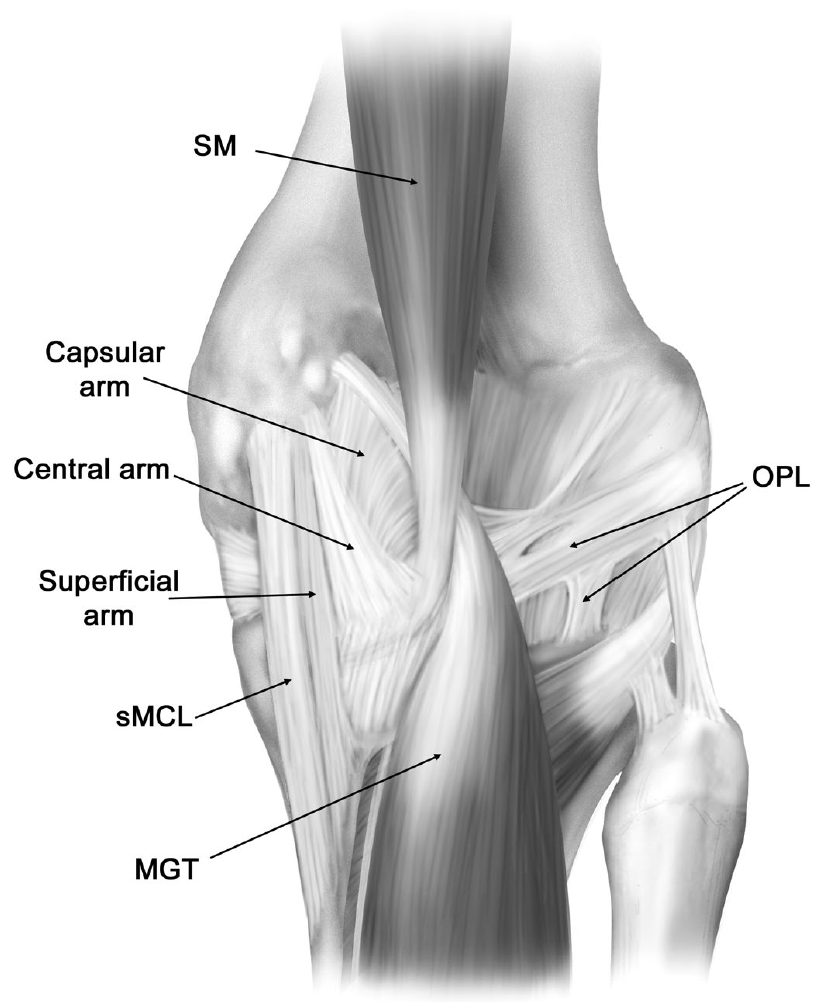
The superficial MCL, as originally described by Brantigan and Voshell7 in 1943, consists of anterior fibers running longitudinally across the joint line which fan out as an oblique array of fibers posteriorly. This posterior portion, running distally and posteriorly at a 25 degree angle to the anterior fibers, was later described as a distinct ligament from the superficial MCL and termed the posterior oblique ligament by Hughston and Eilers.8 The POL originates just distal and posterior to the adductor tubercle, giving it a distinct origin from the superficial MCL, which originates just proximal and posterior to the medial femoral epicondyle.9-11 Distally, the POL has been found to have three readily identifiable arms: the superficial, central, and capsular arms (Figure 2). The central, or tibial arm, is the largest and thickest of the three arms and forms the main portion of the POL, comprising the majority of the ligament’s femoral attachment. Distally, the central arm merges with and reinforces the posteromedial joint capsule, adhering to the posteromedial aspect of the medial meniscus and the adjacent aspect of the tibia at the posterior articular surface. LaPrade9 has suggested that the central arm of the POL appears to be the main structure needed to be repaired or reconstructed in this area following injury to the posteromedial corner of the knee.
Semimembranosus Tendon and its Expansions
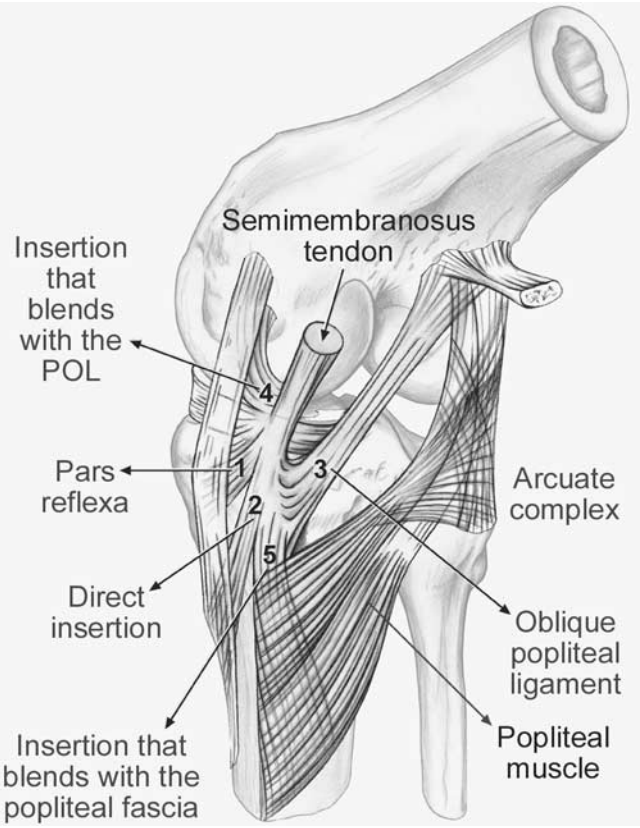
The PMC was described by Müller12 as the “semimembranosus corner” due to the functionally significant contribution of the tendon to the dynamic stability of the knee. Five major arms or expansions have been described: (1) the direct arm (primary attachment), (2) the anterior or reflected arm, (3) the capsular arm, (4) the extension to the OPL (OPL insertion), and (5) the inferior or popliteal arm (Figure 3).
The main tendon bifurcates into two structures, the direct and anterior arms, just distal to the joint line to insert on the posteromedial and medial aspects of the tibia, respectively. The direct arm is the primary attachment of the tendon to the tibia, inserting in a small groove just distal to a tubercle on the posteromedial part of the tibia called the tuberculum tendinis, posterior to the medial tibial crest. The anterior arm, also referred to as the pars reflexa, passes deep to the POL and attaches to the tibia just distal to the medial joint line, deep to the proximal tibial attachment of the superficial MCL in an oval-shaped pattern.9, 13, 3
Oblique Popliteal Ligament (OPL)
The OPL is a broad fascial band, difficult to distinguish from the posterior joint capsule, crossing the posterior aspect of the knee. Arising from the capsular arm of the POL and the lateral expansion of the semimembranosus tendon, it extends from the main portion of the semimembranosus tendon laterally and proximally toward the lateral femoral condyle. As a result, it is considered part of both the PMC and the posterolateral corner. Laterally, the OPL attaches to the meniscofemoral portion of the posterior capsule, to an osseous or cartilaginous fabella, and to the plantaris muscle.14
Posteromedial Joint Capsule
As per Warren et al’s4 three-layered approach to the medial structures of the knee, the joint capsule comprises Layer III along with the deep MCL. LaPrade9 described the deep MCL as a thickening of the medial joint capsule that was most distinct along its anterior border, where it roughly paralleled the anterior aspect of the superficial MCL. Posteriorly, the deep MCL blends with and becomes inseparable from the central arm of the POL, the distinct posterior aspect of the superficial MCL. The central arm forms a thick fascial reinforcement of both the meniscofemoral and meniscotibial portions of the posteromedial capsule, with an additional stout attachment to the medial meniscus.
Posterior Horn of the Medial Meniscus.
The posterior horn of the medial meniscus is intimately linked to various structures of the PMC, including the posteromedial capsule or deep MCL, the POL, and the semimembranosus expansion. These relationships are critical to the dynamic stability of the medial side of the knee, and should be recognized as a “cascade-type” system, where the function of each structure is dependent on the other surrounding structures to which is it attached.5, 13 Furthermore, the stabilizing function of the medial meniscus is of vital importance in the setting of ACL- and PCL-insufficiency.
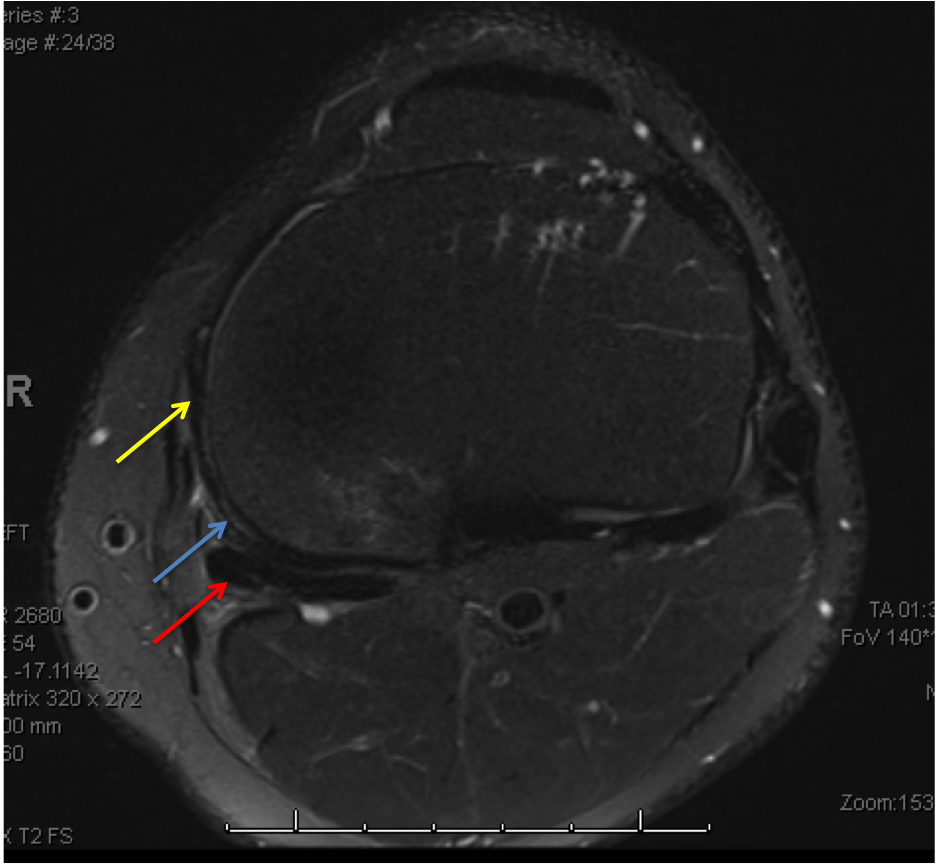
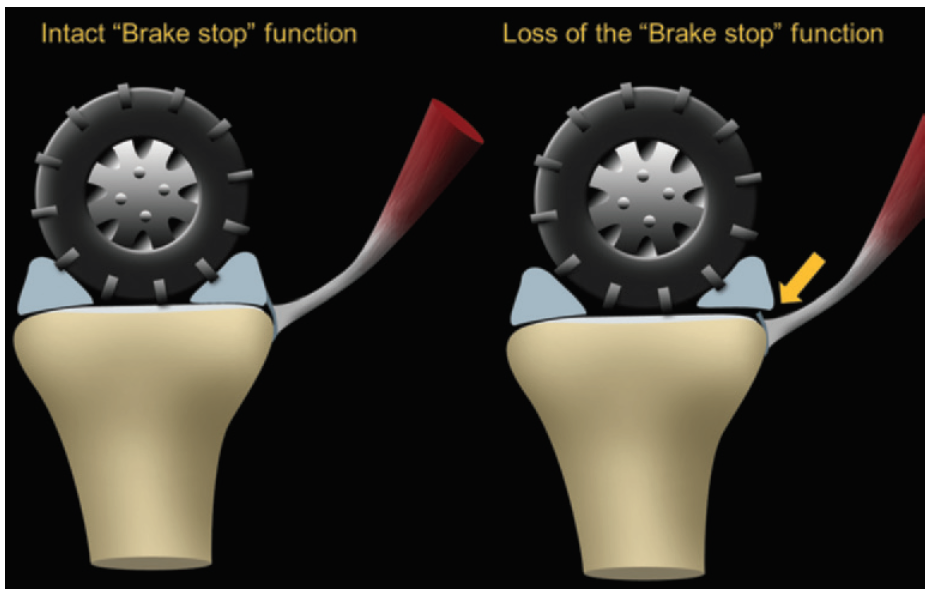
The meniscotibial portion of the deep MCL is an important stabilizer of the medial meniscus on the tibial plateau, with the posterior horn acting in a “brake stop” function to resist anterior tibial translation by engaging the posterior femoral condyle. Injury to the meniscotibial portion of the deep MCL will result in meniscal instability and place the other structures of the PMC under increased stress and prone to injury as the brake stop function is lost (Figure 4). MRI can readily detect injury to both the meniscotibial and meniscofemoral portions of the deep MCL.15 A recent biomechanical cadaveric study has illustrated the importance of the meniscotibial ligament to the rotational stability of the knee and it’s support, along with the posterior horn of the medial meniscus, of the ACL.16
Injury Patterns & Classification
Recent studies have demonstrated several basic patterns of PMC injuries. The POL is the most commonly injured structure. Injury patterns may include sprains, partial tears, and complete tears and are best visualized on axial and coronal MR images.3, 22 Sims and Jacobson5 evaluated a cohort of patients with clinical or functional anteromedial rotatory instability and found injury to the posterior oblique ligament (POL) in 99% of knees studied. The authors reported 3 major injury patterns: (1) POL injury and associated injury to the capsular arm of the semimembranosus (2) POL injury and complete peripheral meniscal detachment and (3) POL injury and disruption of the semimembranosus and peripheral meniscal detachment. The authors also found a high prevalence of associated knee injuries (88%).
Injuries to the semimembranosus tendon may include avulsion fractures, complete or partial tears of the tendon, and chronic insertional tendonitis. Avulsion of the posteromedial plateau occurs during knee flexion with abduction and external rotation of the leg. The insertion site of the direct tibial arm of the tendon is most commonly involved in posteromedial tibial avulsion fractures. Chan et al17 found a 100% incidence of ACL tears in a review of 10 patients with posteromedial plateau injuries and suggested that avulsion fractures at this site may be predictive of concomitant ACL injury.
Meniscocapsular injury can result in disruption, thickening, or bony avulsion of the meniscotibial and meniscofemoral attachments. These lesions are most easily identified on sagittal plane MRI.15 A “reverse Segond fracture” is a bony avulsion at the level of the meniscotibial ligament insertion and has been described by Escobedo et al as occurring in association with PCL rupture.18
Posteromedial corner injuries are most commonly found in association with other ligamentous knee injuries. A study by Halinen et al19 demonstrated that nearly all (22/23) patients surgically treated for combined ACL and MCL injuries had POL tears and 8/23 had total PMC ruptures. Medial sided injuries, including injury to the PMC, have also been demonstrated to be more common than lateral sided injuries with combined ACL-PCL ruptures.20 Chahal et al21 recently evaluated the injury patterns to the posteromedial corner of the knee present in high-grade multiligamentous knee injuries and demonstrated that injury to at least one structure within the PMC was observed in 81% of dislocated knees evaluated. Interestingly, the authors found that injury to the PMC of the knee occurred more frequently than MCL injury alone. Therefore, the presence of multiligamentous knee injuries should raise a high clinical suspicion for PMC lesions.
Clinical Evaluation
History
A thorough history is essential to determine the nature and mechanism of injury, as well as to identify concurrent pathology. Patients will typically describe a valgus force to the affected knee, most commonly occurring during athletic activity. Noncontact injuries usually result in low-grade sprains, whereas a direct blow to the lateral leg produces a significant valgus force and a higher-grade injury. A pure valgus force often causes an isolated MCL injury. Combined external rotation and valgus forces are likely to result in injury to the POL and other components of the PMC. Patients may describe hearing a “pop” and experiencing knee instability with subsequent ambulation. A report of knee dislocation should also increase suspicion for injury to PMC as previously stated.
Physical Examination
The presence of anteromedial rotatory instability (AMRI) on physical exam is the hallmark of PMC injury. Slocum and Larsen22 first described the term AMRI in 1968 as excessive valgus motion with external rotation of the leg. AMRI is clinically characterized by anterior subluxation of the anteromedial tibial plateau on the femoral condyle.23, 24 The presence of AMRI may be tested by applying a valgus stress at 30 degrees of knee flexion while the foot is concomitantly externally rotated. Holding the limb by the plantar surface of the foot instead of the distal leg allows for appreciation of the rotatory component.25 A positive test occurs with medial joint space gapping and anterior subluxation of the medial tibial plateau relative to the femur. The positive exam correlates with a combined PMC and MCL injury. The anteromedial drawer test is also used to evaluate for AMRI. This test is performed by flexing the knee to 90 degrees while externally rotating the foot 10-15 degrees and applying an anterior force to the knee. Anteromedial tibial plateau subluxation is a positive test and is indicative of injury to the PMC.
Additional ligamentous exams should include valgus stress testing and posterior drawer testing. Valgus stress testing should be performed at 0 and 30 degrees of knee flexion to assess the integrity of the MCL. It is important to differentiate isolated MCL injury from AMRI, by assessing for valgus laxity associated with anterior rotatory subluxation of medial tibial plateau on the medial femoral condyle with the AMRI pattern.26 Posterior drawer examination should be performed with the tibia in neutral and internal rotation for suspected PCL injury. In an isolated PCL injury there will be decreased posterior tibial translation with the tibia in internal rotation due to the POL and posteromedial capsule functioning as secondary stabilizers to posterior tibial translation.20, 27, 28 Therefore, in combined PCL-PMC injuries there will be equal posterior translation of the tibia relative to the femur with the tibia in both neutral and internal rotation.
Imaging
Imaging studies are critical for the diagnosis of PMC injuries, particularly in the setting of an acute injury when a thorough exam is not possible or equivocal due to patient guarding. A standard radiographic series is the initial step in the evaluation of suspected PMC injuries. The series should include anteroposterior (AP), lateral, and oblique views. Standing radiographs are useful to assess overall limb alignment, but are not always practical due to pain with weight bearing. Although plain radiographs are frequently normal, they may demonstrate avulsion fractures or osteochondral defects. Radiographs should be carefully evaluated for any evidence of joint space narrowing or asymmetry, raising suspicion for knee dislocation and multiligamentous injuries.
Objective evaluation of knee laxity may be performed with stress radiographs of the knee. LaPrade et al29 developed a quantitative method of analyzing valgus knee radiographs. In a biomechanical study the authors found that >3.2mm of laxity compared with the contralateral knee at 20-degrees of flexion is indicative of a grade-III MCL lesion. Significant gapping at 0-degrees and 20-degrees (up to 9.8mm) was found to correlate with complex knee injuries involving MCL, posteromedial corner, and cruciate ligaments. Posterior stress films may also be performed to assess combined injuries. Garavaglia et al30 found >9mm of posterior tibial translation with posterior stress views at 30-degrees of knee flexion and >12mm at 80-degrees of knee flexion were indicative of PCL and associated lesions (LCL, MCL, PMC, PLC).
Magnetic resonance imaging (MRI) is the current imaging modality of choice for diagnosing the complex injuries of the PMC. Many of the normal anatomic components of the PMC are difficult to visualize on MRI due to their thin profile and close proximity to surrounding structures. In a cadaveric study, Loredo et al31 found these structures challenging to identify on MRI, but found slight improvement in visualization with contrast-enhanced sequences and coronal oblique images. Recognizing edema and soft tissue thickening can identify many injuries of the PMC. Additionally, MRI allows for the evaluation of associated injuries within the knee and assists with pre-operative planning.
Surgical Management
There are various techniques described regarding repair or reconstruction of the posteromedial structures of the knee, each demonstrating acceptable clinical results32-35. In our experience, injuries that involve the PMC typically occur in patients with multiligamentous injuries or in those that sustain knee dislocations. Isolated, low-grade medial knee injuries that involve the MCL and posteromedial corner can be treated non-operatively, however those with tibial-sided avulsions that include a sleeve of tissue encompassing both the MCL and posteromedial corner may benefit from early fixation. Chronic PMC injuries where patients have developed symptomatic AMRI are considered for surgical reconstruction. We routinely obtain standing pre-operative leg length radiographs, as patients with significant valgus deformity should be considered for corrective osteotomy.
We recommend a thorough examination under anesthesia and diagnostic arthroscopy regardless of which method of surgical management is chosen. During the initial arthroscopy, meniscal pathology should be addressed, the articular cartilage should be assessed, and an intra-operative stress examination should be performed. Our preferred approach, if the soft tissues allow, is to perform an acute reconstruction of the cruciates (in the case of a combined ACL/PCL injury) with medial repair versus reconstruction, depending on the quality of the medial tissues.
Repair
Surgical repair of PMC injuries has been shown to be an effective treatment option to restore knee stability and improve functional outcomes36, 37 Often, the MCL must be repaired in conjunction with the PMC. A medially based longitudinal incision extending from the level of the superior patella and extending 6-8 centimeters distal to the joint line should be utilized and soft tissue dissection taken down to the superficial MCL and posteromedial structures. Care is made to protect the hamstring insertions at the pes anserine. Fixation can be accomplished with several options, including suture anchors, staples, or screw-and-washer type constructs. Whichever fixation method is chosen, we recommend approaching these injuries in a deep-to-superficial fashion. The medial meniscus and meniscocapsular attachments should be approached first. The meniscotibial attachments can be repaired with small suture anchors placed around the surface of the tibia from posterior to anterior, just distal to the tibial articular surface, taking care not to violate the articular cartilage. Suture anchor repair can be used for tibial or femoral-sided avulsions of the POL, assuming the tissue is of robust quality. Advancement of the tissue and re-approximation into the superficial MCL has also been described.38 The semimembranosus should be evaluated, and, if torn, can be advanced and sutured into the superficial MCL tissue in a pants-over-vest fashion or re-attached with a suture anchor. We feel this is important to recognize given this tendon’s role in dynamic stabilization of the knee.
Clinical results following surgical repair have generally been good. DeLong and Waterman recently conducted a meta-analysis of patients undergoing repair of medial collateral ligament and posteromedial corner injuries and found that in 93 knees, the mean side-to-side difference in medial joint space opening was 1.25mm. In total, 6.1 percent of knees met criteria for failure of the repair.33
In contrast, Stannard et al described their cohort of patients who sustained knee dislocations with multiligamentous injuries and found a lower failure rate in those patients that underwent reconstruction rather than repair. The authors reported that 80% of their patients who underwent direct repair of the PMC achieved post-operative valgus stability compared to 96% of those treated with surgical reconstruction. 36
Reconstruction
In the case of chronic, symptomatic rotatory instability (AMRI), valgus instability (especially in full extension), or posterior instability with PMC and PCL insufficiency, surgical reconstruction should be considered. Multiple methods of reconstruction have been described in the literature, and choice of graft is based on the surgeon’s preference and experience. Generally, in the cases of multi-ligamentous knee injuries, we prefer the use of allograft tissue to limit donor site morbidity. PMC reconstruction has been described using a variety of different techniques, all of which have shown promising results. 34, 32, 35, 39
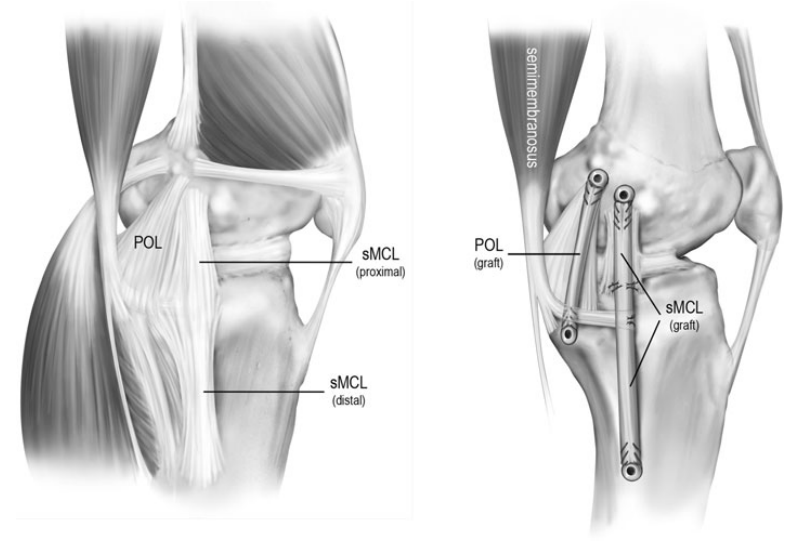
Our preferred technique for PMC reconstructions is that described by Laprade and Wijdicks35, which is an anatomic reconstruction of the proximal and distal divisions of the superficial MCL and the POL using two separate grafts (Figure 5). An anteromedial longitudinal incision beginning 4 centimeters medial to the patella and extending 8 centimeters distal to the joint line is utilized to expose both the femoral the distal tibial attachment sites of the superficial MCL. The sartorial fascia is incised to expose the gracilis and semitendinosus tendons. The semimembranosus tendon can be harvested for autograft based on surgeon preference. Deep within the pes anserine bursa, the distal tibial attachment of the superficial MCL can be identified, 6 centimeters distal to the joint line. First, a reconstruction tunnel is created for the superficial MCL. A guide pin is placed from medial to lateral at the posterior aspect of the superficial MCL’s tibial insertion and a 6- or 7-millimeter tunnel is reamed to a depth of 25 millimeters. A reconstruction tunnel for the central arm of the POL is then placed just anterior to the direct arm attachment of the semimembranosus tendon. A guide wire is placed, erred towards Gerdy’s tubercle and over-reamed with a 6 or 7mm reamer to a depth of 25 millimeters.
Attention is then turned towards the femoral tunnel sites. If the femoral attachment sites of the native POL and MCL are not readily visualized from the injury pattern, one can estimate the tunnel locations by using bony topography. The superficial MCL tunnel is placed slightly proximal and anterior to the medial epicondyle. The femoral POL tunnel is placed approximately 8mm distal and 3mm anterior to the gastrocnemius tubercle. It is recommended to identify both tunnel sites before reaming, rather than reaming each tunnel individually, in order to decrease the possibility of reaming a tunnel outside the ideal location. Guide pins are placed across the femur and once tunnel position is confirmed to be acceptable, a 6- or 7-millimeter reamer is used to drill each reconstruction tunnel to a depth of 25 millimeters. The femoral ends of the grafts are first fixed with interference screws. The POL graft is then placed into its tibial tunnel and tensioned in full extension and neutral rotation. The superficial MCL is weaved under the sartorial fascia and fixed in its tibia tunnel with the knee held in neutral rotation, 20 degrees of flexion, and a slight varus reduction force to ensure no medial compartment gapping. Attention is then directed towards re-creating the proximal tibial attachment site of the superficial MCL graft. A suture anchor is placed 12-13 millimeters distal to the medial joint line, just anterior to the anterior arm of the semimembranosus tendon attachment. The superficial MCL graft is secured to this site with the anchor, restoring the native proximal tibial attachment.
In patients undergoing concomitant PCL reconstruction via femoral bone tunnels, it is important to position the superficial MCL and POL tunnels aiming 30 degrees proximally and anteriorly (in the coronal and axial planes, respectively). Tunnels drilled at 0 degrees in the axial plane may result in shorter tunnels and an increased risk of intersection with a PCL femoral tunnel.40 In the case of a multi-ligamentous reconstruction, we typically tension the cruciates before tensioning the collateral ligaments.
In their series of 28 patients, with an average of 1.5 years of follow up, Laprade and Wijdicks noted vast improvement in IKDC scores, elimination of side-to-side instability in all patients, and an average of 1.3mm of increased gapping on stress radiographs compared to the contralateral knee.
Two alternative techniques utilizing the native semitendinosus tendon have been described, keeping the distal insertion of the tendon intact.32, 34 Both have demonstrated promising results.
Conclusion
Our understanding of the posteromedial corner has significantly increased over recent years. Novel anatomic and biomechanical studies demonstrate the PMC to be an important primary stabilizer of valgus laxity and a secondary stabilizer to anterior tibial translation and external rotation. Anteromedial rotatory instability (AMRI) is the hallmark of PMC injuries and one must have a high index of suspicion for such injuries, as PMC injuries are a likely cause of chronic valgus laxity and late graft failure after ACL reconstruction. Limited studies of PMC injuries treated with primary repair or reconstruction of the superficial MCL and POL have resulted in good functional outcomes and low failure rates. Further research regarding short and long-term outcomes after surgical treatment for PMC injuries is warranted.
To schedule an appointment with Dr. Dold, click here. A member of our team will be in contact with you soon – usually within an hour of receiving your request if within regular business hours.