*IMPORTANT: Contact us immediately if you have been diagnosed with or suffered an acute patella (or quadriceps) tendon rupture. Ideally, surgical repair of the tendon should take place within two (2) weeks of the initial injury. To schedule an appointment with Dr. Dold, click here. A member of our team will be in contact with you soon – usually within an hour of receiving your request if within regular business hours.*
The diagnosis of quadriceps and patellar tendon ruptures requires a high index of suspicion and thorough history-taking to assess for medical co-morbidities that may predispose patients to tendon degeneration. Radiographic assessment with plain films supplemented by magnetic resonance imaging (MRI) when the work-up is equivocal further aids diagnosis. Advanced imaging is often unnecessary in patients with functional extensor mechanism deficits. Acute repair is preferred, and transpatellar bone tunnels serve as the primary form of fixation when the tendon rupture occurs at the patellar origin, with or without augmentation depending on the injury and quality of the tendon and the primary repair. Chronic tears and disruptions following total knee arthroplasty are special cases requiring reconstructions with allograft, synthetic mesh, or autograft. Rehabilitation protocols generally allow immediate weight-bearing with the knee locked in extension and crutch support. Limited arc motion is started early with active flexion and passive extension and then advanced progressively, followed by full active range of motion and strengthening. Complications are few but include quadriceps atrophy, knee stiffness (arthrofibrosis), and re-rupture. Outcomes are excellent if repair is done acutely, with poorer outcomes associated with delayed repair. Thus, it is important to seek surgical consultation as soon as the injury is suspected.
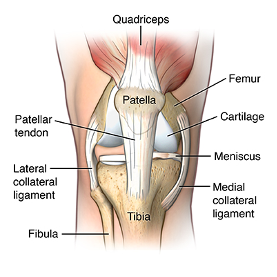
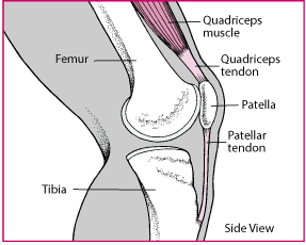
Anatomy
The patellar tendon is key component in the extensor mechanism of the knee. The entire mechanism is composed of the quadricep muscle, quadricep tendon, patella, patellar tendon, and the tibial tubercle located on the proximal tibia. The patellar tendon is located at the distal portion of this mechanism. It originates from the inferior pole of the patella and courses distally to attach at the tibial tubercle. The dimension of the patellar is approximately 30mm wide and 50mm long, but varies slightly from patient to patient based on body habitus and size. The thickness of the tendon can range from 5mm to 7mm. The patellar tendon helps connect the quadriceps muscle to the lower leg at the tibial tubercle which allows the lower leg to move from flexion to extension.
Etiology
Patellar tendon ruptures are usually associated with chronic tendinosis of the patellar tendon but can occur as isolated, traumatic injuries in the setting of a noraml tendon. Chronic tendinosis, if left untreated, can ultimately lead to weakening of the tendon which can cause catastrophic failure of the patellar tendon under significant stress. There can be multiple systemic medical conditions or underlying factors that can contribute to weakened tendons such as chronic overuse, systemic lupus erythematosus, rheumatoid arthritis, diabetes, chronic steroid use (seen in many treatments plans for systemic diseases), or corticosteroid injections into the patellar tendon itself which can lead to tendon damage. The extensor mechanism can fail anywhere in the chain. Most commonly they occur within the patella itself with a fracture. Quadricep tendon rupture affects approximately 1.3% of patients and patellar tendon ruptures affect approximately 0.5% of patients. Patellar tendon ruptures most commonly occur in men more than women at a 2:1 ratio and more commonly occur in the 3rd or 4th decades of life.
Pathogenesis
Rupture of the patellar tendon typically occurs due to an overload of the tensile forces across the extensor mechanism. This overloading of the tendon that leads to failure is secondary to longstanding tendinosis and chronic inflammation of the tendon. This failure of the tendon usually occurs with the knee in a flexed position as most of the force is placed across the tendon with the knee placed in more than 60 degrees of flexion. With the most force across the tendon being in a flexed position beyond 60 degrees, jumping sports typically see patellar tendon ruptures due to the knee placed in repetitive flexion with large forces placed across the tendon. The rupture most commonly occurs at the proximal aspect of the patellar tendon at the inferior pole of the patella, but it could rupture within the tendon itself or at the distal aspect at the tibial tubercle. With the most common location being the inferior pole of the patella, you can have rupture with or without a bony avulsion of the patellar tendon.
Presentation
The patient will most likely present with a large knee effusion and the inability to bear weight or perform a straight leg raise of the affected leg (the extensor mechanism of the leg is no longer in continuity and the patient is unable to extend the knee or perform an SLR). The patient may report hearing a pop within the knee with a sudden “giving out” sensation of the knee. On inspection of the knee you can often see a large effusion with acute ruptures and can sometimes palpate a void at the inferior pole of the patella where the tendon originates from the boney patella. The extensor mechanism must be tested if a patellar tendon rupture is suspected. If a patella tendon rupture is present, the patient will be unable to actively extend the lower leg or perform a straight leg raise. Physical examination is vital to an accurate diagnosis.
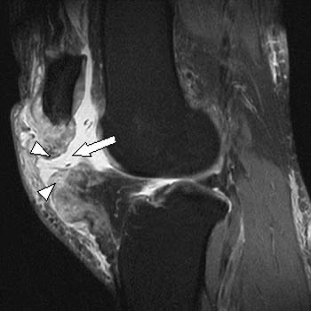
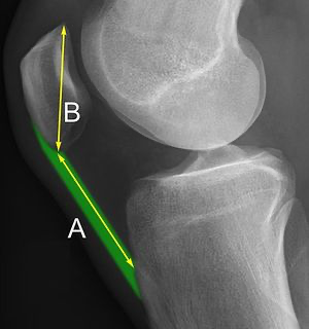
Imaging
Upon suspicion of a patellar tendon rupture, the initial imaging study will be a plain film radiograph with an AP and lateral view. Plain films will reveal a high riding patella in relation to the femur, which is known as radiographically as “patella alta.” You can classify the degree of patella alta with the Insall – Salvati ratio which measures the length of the patella and the length of the patellar tendon. A normal ratio is between 0.8 and 1.2, above 1.2 is considered patella alta and a patellar tendon rupture should be suspected. With most of the patellar tendon ruptures occurring at the inferior pole of the patella, plain radiographs can help identify avulsion fractures from the inferior pole of the patella. The next study that will be ordered is an MRI of the knee to correctly diagnose and assess the degree of rupture within the patellar tendon. MRI can identify the exact location of the rupture as well as any other additional soft tissue pathology within the knee such as meniscus damage or ligamentous injuries.
Treatment
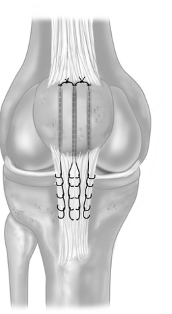
Treatment is aimed at restoring the extensor mechanism as it plays a vital role in daily activities. Open patellar tendon repair is the go-to procedure for a patellar tendon rupture. This helps restore the extensor mechanism and regain function of normal activity. The location of the rupture can help dictate which technique is utilized. With the most common location being the inferior pole of the patella, bone tunnels will often be utilized to help bring the tendon back to its origin at the inferior pole of the patella. However, new studies show that use of suture anchors for proximal tendon repair has shown favorable outcomes in both re-rupture rate and a decreased gap formation when compared to transosseous tunnels. A mid-substance rupture will typically involve an end-to-end repair with sutures to re-approximate the tendon ends. If the rupture is more distal, suture anchors can be utilized to help reattach the distal tendon to the tibial tubercle. Postoperatively, weight bearing will begin with the knee locked in full extension. It is the upmost importance to protect the repair at all costs with strict protocol to gradually increase range of motion within the affected knee. Full range of motion should be achieved by the 3-month mark post-operatively.
Related Research
- Traumatic Patellar Tendon Rupture Repair Using Synthetic Ligament Augmentation.
- Quadriceps and patellar tendon ruptures.
- Platelet-rich plasma in tendon-related disorders: results and indications.
- Surgical treatment options for patella tendon rupture, Part I: Acute.
- Patellar Tendon Rupture Bedside Diagnosis.
- Patella tendon rupture after arthroscopic resection of the prepatellar bursa–a case report.
- Bilateral Patellar Tendon Rupture.
- Rethinking Patellar Tendinopathy and Partial Patellar Tendon Tears: A Novel Classification System.
- Treatment of Chronic Patellar Tendon Rupture with Hamstrings Tendon Autograft.
- Reconstruction of chronic patellar tendon rupture with contralateral bone-tendon-bone autograft.
- Repair of Acute Patellar Tendon Rupture Augmented with Strong Sutures.
- Rupture of the quadriceps tendon: an association with a patellar spur.
- Regarding “Rupture of the Patellar Tendon after Platelet-Rich Plasma Treatment: A Case Report”.
- Traumatic patella tendon rupture: early mobilisation following surgical repair.
- Adult native knee extensor mechanism ruptures.
- Reconstruction of a chronic patellar tendon rupture with semitendinosus autograft.
- Extensor mechanism ruptures.
- Acute traumatic rupture of the patellar tendon in pediatric population: Case series and review of the literature.
- Surgical options for chronic patellar tendon rupture in total knee arthroplasty.
- Surgical Treatment for Failure of Repair of Patellar and Quadriceps Tendon Rupture With Ipsilateral Hamstring Tendon Graft.
- Better knee function after surgical repair of acute quadriceps tendon rupture in comparison to acute patellar tendon rupture.
Contact us immediately if you have been diagnosed with or suffered an acute patella tendon rupture. Ideally, surgical repair of the tendon should take place within two (2) weeks of the initial injury. To schedule an appointment with Dr. Dold, click here. A member of our team will be in contact with you soon – usually within an hour of receiving your request if within regular business hours.